2 Minute Medicine Rewind April 3, 2017
Recent studies have shown that the introduction of eggs early on in the diet is associated with reduced egg allergy. Infant feeding guidelines are also shifting to recommend that traditionally allergenic foods be included in the infant diet from as early as 4-6 months of age. In this double-blind randomized controlled trial, 820 infants were randomized to receive daily egg powder from 4 to 6.5 months or a color- and texture-matched rice powder up to 10 months of age with the aim of assessing the risk reduction in egg allergy achieved through early introduction of eggs in the diet. Researchers found that there was a 25% risk reduction in egg allergy with early regular egg intake compared to egg avoidance up to 10 months. This finding, however, was not statistically significant. The authors also performed exploratory analyses to determine whether the effect of treatment was modified by maternal, family or infant characteristics. The results of these analyses showed that socioeconomic status (SES) modified the effect of early regular egg introduction, with the intervention having less effect in higher SES families when compared to lower SES families (RR 0.47, 95% CI 0.27 to 0.84, interaction P = 0.02). Total household egg intake also modified the effect of early regular egg consumption, with treatment decreasing the risk of egg allergy in families who ate less than 12 eggs per week, but not in families who ate 12 or more eggs per week (RR 0.36, 95% CI 0.16 to 0.82, interaction = 0.04). This study therefore shows that infants from families of higher SES and those who consume fewer eggs per week are most likely to benefit from early regular egg intake.
Patients diagnosed with type 1 diabetes mellitus require lifelong administration of insulin to regulate blood glucose levels and minimize the risk of macrovascular and microvascular complications. Generally, insulin is administered by multiple daily subcutaneous injections, using different types of insulins in order to meet background and meal requirements. Doses are adjusted according to intake, physical activity and blood glucose levels. However, many patients struggle to achieve optimal glycemic targets. In continuous subcutaneous insulin infusion, quick-acting insulin is delivered under the skin by means of a pump, supplying insulin to meet both background and meal-related requirements. This method has been associated with improved glucose control, reduced risk of hypoglycemia and enhanced quality of life when compared to multiple daily injections. However, recent studies have indicated that patients using continuous subcutaneous insulin infusion receive more training and attention in managing blood glucose levels than those using multiple daily injections. As such, in this randomized controlled trial, 317 patients were randomized to receive training in the use of pump or multiple daily injections to compare the effectiveness of insulin delivery methods in the setting of equivalent training in flexible insulin treatment. Researchers found that at 24 months of follow-up, in patients whose baseline hemoglobin A1c (HbA1c) was 7.5% of greater, the mean change in the pump group was 0.85% compared to 0.42% in the multiple daily injections group (mean difference -0.24%, 95% CI -0.53% to 0.05%, p=0.10). There was no statistically significant difference in the proportion of patients reaching an HbA1c of 7.5% or less in each of the groups after 2 years of follow-up. There was also no significant difference in the incidence of severe hypoglycemic episodes (RR 1.13, 95% CI 0.51 to 2.51). This study therefore shows that in the setting of equivalent training, there is no significant difference between multiple daily injection and continuous subcutaneous infusion of insulin in terms of blood glucose control.
Rivaroxaban or aspirin for extended treatment of venous thromboembolism
Venous thromboembolism (VTE) is treated with the use of direct oral anticoagulation agents, such as rivaroxaban, or vitamin K antagonists, such as warfarin. Anticoagulation therapy is therapy is typically administered for 3 months or longer, depending on the patient’s risk of recurrent VTE along with their risk of bleeding. In patients at risk of recurrent VTE, extended anticoagulation therapy is effective in the prevention of repeat episodes. However, given the increased risk of bleeding, there is a reluctance to continue anticoagulation beyond 6 to 12 months. Attempts to reduce the risk of bleeding when treatment is extended include the use of lower-dose anticoagulant therapy and the use of aspirin in place an anticoagulant. In this randomized controlled trial, 3365 patients were randomized to receive either once-daily rivaroxaban (at doses of 20 mg or 10 mg) or 100 mg of aspirin to compare the efficacy of these pharmacologics in preventing symptomatic recurrent fatal or non-fatal VTE, as well as the risk of bleeding associated with use of these medications. Researchers found that patients were significantly less likely to experience symptomatic recurrent VTE if receiving 20 mg rivaroxaban (HR 0.34, 95% CI 0.20 to 0.59, p<0.001) or 10 mg rivaroxaban (HR 0.26, 95% CI 0.14 to 0.47, p<0.001) as opposed to aspirin. There was no statistically significant difference in the risk of symptomatic recurrent VTE between the 10 mg and 20 mg rivaroxaban groups. There were also no statistically significant differences between any of the groups with respect to the incidence of major or non-major bleeding. This study therefore shows that in patients with VTE requiring long-term anticoagulation, the risk of recurrent VTE is significantly reduced with the use of rivaroxaban as opposed to aspirin, without a significantly increased risk of bleeding.
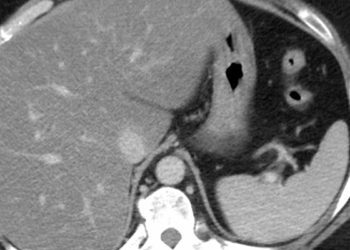
Cigarette smoking and pancreatic cancer survival
Cigarette smoking is associated with an increased risk of pancreatic cancer, contributing to the development of approximately 20% of cases. Few studies, however, have assessed the effects of cigarette smoking on pancreatic cancer survival. In this retrospective cohort study, 485 pancreatic cancer patients were followed up to assess the effect of cigarette smoking on pancreatic cancer survival. Researchers found that current smokers had a reduced survival rate compared to never smokers (HR 1.37, 95% CI 1.11 to 1.69, p =0.003). In considering the more immediate impact of smoking on perioperative mortality in patients undergoing surgical resection of their cancer, the authors also repeated the analysis with the exclusion of patients with localized disease. This adjustment, however, did not change the results considerably (HR 1.43, 95% CI 1.14 to 1.79). The association between cigarette smoking and survival also persisted with adjustment of comorbidities (HR 1.31, 95% CI 1.04 to 1.65). The authors also found a negative trend in survival with increasing pack-years of smoking, where the survival rate was lower in patients with a smoking history in excess of 60 pack-years (HR 1.49, 95% CI 1.05 to 2.10) compared to those with a smoking history of 1 to 30 pack-years (HR 1.32, 95% CI 1.00 to 1.75). Possible associations between prediagnostic circulating levels of cotinine, a metabolite of nicotine that is proportional to tobacco smoke exposure, and survival were also studied. Researchers found that heavy smokers as defined by prediagnostic circulating cotinine levels had a significantly reduced survival rate compared to non-smokers (HR 2.47, 95% CI 1.24 to 4.92). This study therefore shows that cigarette smoking is associated with a reduction in survival among patients with pancreatic cancer.
Risk of firearm injuries among children and youth of immigrant families
Firearm injuries are a source of substantial morbidity and mortality among children and youth. Risk factors for sustaining a firearm injury or being a victim of homicide include young age (<5 years), late adolescence, male sex, low socioeconomic status (SES), Indigenous ethnicity, black race, access to a firearm in the home, and involvement in a gang. One other group potentially at-risk includes immigrant children and youth. While it has been observed in some studies that, despite social disadvantage, new immigrants have better health outcomes than native-born individuals, this phenomenon has not been consistently observed among children or well-studied among victims of violent crime or unintentional firearm injuries. In this population-based cohort study, 20,418,245 residents of Ontario, Canada age 24 years and younger were followed up to describe the epidemiology of victims of unintentional and assault-related firearm injuries among immigrant children and youth. Researchers found that male nonimmigrants had 1032 unintentional (12.4 per 100,000, 95% CI 11.7 to 13.2) and 304 assault-related (3.6 injuries per 100,000, 95% CI 3.2 to 4.0) firearm injuries. This is in contrast to male immigrants who had 148 unintentional (7.2 per 100,000, 95% CI 6.1 to 8.5) and 113 assault-related (5.5 per 100,000, 95% CI 4.5 to 6.6) firearm injuries. Female nonimmigrants had 137 unintentional (1.7 per 100,000, 95% CI 1.4 to 2.0) and 31 assault-related (0.4 per 100,000, 95% CI 0.3 to 0.5) firearm injuries. Female immigrants had 12 unintentional and less than 6 assault-related firearm injuries. Researchers also found that the risk of unintentional firearm injury was lower among immigrant children and youth (RR 0.5, 95% CI 0.4 to 0.6). The risk of assault-related firearm injury was not associated with immigrant status. In assessing the risk of firearm injury in relation to immigration characteristics, the authors found that refugees were at an increased risk of assault-related firearm injury (RR 1.4, 95% CI 1.0 to 2.0). In addition, the risk of assault-related firearm injury was higher among long-term immigrants living in Canada for over 10 years, compared with nonimmigrants (RR 1.35, 95% CI 1.10 to 1.66), with rates of injury particularly high among immigrants from Africa (RR 2.8, 95% CI 2.0 to 4.1) and Central America (RR 4.1, 95% CI 3.0 to 5.6). This study therefore shows that compared to nonimmigrants, immigrant children and youth had a lower risk of unintentional firearm injury. The risk of assault-related firearm injury, however, was increased among refugees and immigrants from Africa and Central America, pointing to a need for prevention strategies in these newly identified high-risk groups.
Image: PD
©2017 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.