2 Minute Medicine Rewind August 11, 2025
Discontinuation rates and predictors of Medical Cannabis cessation for chronic musculoskeletal pain
1. Medical cannabis has a high discontinuation rate among patients with chronic musculoskeletal pain, particularly in the first few months, particularly in older patients
2. Pain location and baseline health status are not reliable indicators of whether a patient will continue medical cannabis use.
Evidence Rating Level: 3 (Average)
In this retrospective study, 78 patients with chronic musculoskeletal pain certified for medical cannabis (MC) at a single orthopedic institute between October 2022 and December 2024 were followed for up to one year to assess discontinuation rates and associated factors. Demographics, pain origin, and baseline Patient-Reported Outcomes Measurement Information System (PROMIS) Global Physical Health (GPH) and Global Mental Health (GMH) scores were collected. Discontinuation status was confirmed through follow-up visits and the state MC registry. At three months, 44.7% of patients had discontinued MC, primarily due to dissatisfaction, preference for alternative treatments, or surgical intervention. By one year, 57.9% had ceased use, with older age significantly associated with discontinuation (mean 71.5 vs. 64.5 years; p = 0.04). Pain origin, including low back pain, did not significantly differ between those continuing and discontinuing, and baseline GPH/GMH scores were similar in both groups. These findings suggest that over half of patients stop MC within a year, with older adults more likely to discontinue, and that baseline health status and pain location are not strong predictors of adherence. Further research is warranted to identify modifiable factors that could improve long-term MC use for chronic musculoskeletal pain.
1. Hydroxychloroquine plus prednisolone reduced the 12-month risk of the composite cardiovascular outcome by 72 percent compared with prednisolone alone.
2. Hydroxychloroquine plus prednisolone normalized a wide range of inflammation-related proteins, indicating multiple anti-inflammatory effects.
3. The safety profile was similar to prednisolone alone, with no serious treatment-related adverse events.
Evidence Rating Level: 1 (Excellent)
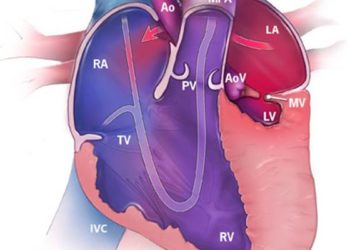
In this multicenter, open-label, evaluator-blinded, randomized phase II trial (HYPIC), 50 adults with chronic inflammatory cardiomyopathy (infl-CMP) following fulminant myocarditis (FM) were randomized to receive either hydroxychloroquine (HCQ) plus prednisolone (PDN) or PDN alone for 12 months, in addition to guideline-directed heart failure therapy. The primary endpoint was a composite of cardiovascular death or heart transplant, hospitalization for heart failure or recurrent myocarditis, and permanent pacemaker or implantable cardioverter-defibrillator implantation. Secondary outcomes included changes in left ventricular ejection fraction (LVEF), left ventricular internal diastolic diameter (LVIDd), high-sensitivity cardiac troponin I (hs-cTnI), NT-proBNP, hs-CRP, and ESR. HCQ + PDN significantly reduced the primary composite outcome versus PDN alone (24.0% vs. 60.0%, HR 0.28, 95% CI 0.11–0.71) and led to greater improvements in LVEF, LVIDd, hs-cTnI, NT-proBNP, and hs-CRP (all p < 0.05). Proteomic analysis showed HCQ + PDN normalized 16 inflammatory proteins compared with only 2 in the PDN group. Adverse events were similar between groups, with no serious drug-related events. The authors conclude that HCQ + PDN for 12 months improves prognosis, cardiac function, and inflammation control in infl-CMP after FM, with acceptable safety, supporting further large-scale trials.
1. Remote monitoring significantly reduced systolic blood pressure (BP) compared to usual care (−2.7 mm Hg, p = 0.002), especially in patients with uncontrolled baseline BP who achieved a 17.7 mm Hg systolic BP reduction.
2. Self-monitoring alone did not improve BP control versus usual care
Evidence Rating Level: 1 (Excellent)
Hypertension management remains a critical challenge, with traditional methods like office-based monitoring and self-monitoring showing limitations in long-term efficacy. This multicenter randomized controlled trial compared the effectiveness of remote monitoring, self-monitoring, and usual care in 1,006 hypertensive patients over 24 months. Participants were assigned to one of three groups: remote monitoring (using a cloud-based system with physician alerts for abnormal readings), self-monitoring (manual logging without remote feedback), or usual care (routine clinical management). The primary outcome was systolic blood pressure (BP) reduction. Results demonstrated that the remote monitoring group achieved significantly greater systolic BP reductions (−2.7 mm Hg vs. usual care, p = 0.002) and higher target BP attainment rates (69.65% at 24 months). Notably, patients with suboptimal baseline BP in the remote group saw a 17.7 mm Hg drop in systolic BP. Self-monitoring alone showed no significant benefit over usual care. The remote group also exhibited increased use of calcium channel blockers, diuretics, and combination therapy, suggesting better medication optimization. The study concludes that remote monitoring with real-time clinician feedback enhances BP control, while self-monitoring without additional support is ineffective.
1. Patients with severely disturbed sleep had the highest comorbidity burden, lowest ejection fraction, and poorest cognitive function.
2. Older age, higher physical symptom burden, and depression were significant predictors of worse sleep quality.
Evidence Rating Level: 1 (Excellent)
Sleep disturbances are highly prevalent in heart failure (HF) patients, affecting nearly 80% of individuals and significantly impairing quality of life and clinical outcomes. This secondary analysis of the MOTIVATE-HF trial used latent class analysis (LCA) to identify distinct sleep quality patterns in 510 Italian HF patients (mean age 72.4 years, NYHA class II–IV) based on Pittsburgh Sleep Quality Index (PSQI) components. Three clusters emerged: (1) Inadequate Sleep (46.1%)—adequate duration but frequent disturbances and daytime dysfunction; (2) Severely Disturbed Sleep (25.3%)—widespread sleep problems with low medication use; and (3) Mildly Disturbed Sleep (28.6%)—minor issues despite mild disturbances. Cluster 2 patients had the worst outcomes, including higher comorbidity burden (mean Charlson Index=3.55), lower ejection fraction (40%), and poorer cognitive function (MoCA=21.5), while Cluster 3 patients were younger with better cardiac and mental health. Predictors of poor sleep included older age, higher symptom burden, and depression. The study underscores the heterogeneity of sleep disturbances in HF and advocates for personalized interventions, such as targeted symptom management and psychological support, integrated into routine HF care to improve sleep quality and overall prognosis.
1. Higher Post-operative Day 1 (POD1) pain scores were independently associated with increased 30-day infectious and non-infectious complications.
2. Infectious complications developed later (mean 6.5 days) than non-infectious complications (4.1 days).
Evidence Rating Level: 2 (Good)
Early postoperative pain is a significant concern following major abdominal surgery, with growing evidence linking its intensity to increased 30-day complication risks. This retrospective cohort study analyzed 1,000 patients undergoing cytoreductive surgery with hyperthermic intraperitoneal chemotherapy (HIPEC), esophageal, liver, or pancreatic surgery at Radboud University Medical Center (2014–2020). Pain scores on postoperative day 1 (POD1) were assessed using the Numeric Rating Scale (NRS), and complications were classified by Clavien-Dindo (CD) criteria. Results revealed 790 complications in 572 patients (36.7% infectious, 63.4% non-infectious), with infectious complications occurring later (mean 6.5 vs. 4.1 days, *p*<0.001). Logistic regression demonstrated that higher POD1 pain scores significantly predicted total complications (OR=1.132), CD severity (OR=1.131), infectious (OR=1.126), and non-infectious complications (OR=1.079). Covariates like age, ASA class, open surgery, and longer duration also contributed. The study highlights the role of early pain in impairing recovery (e.g., reduced mobility, immunosuppression) and underscores the need for optimized perioperative analgesia to mitigate complications.
Image: PD
©2025 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.