2 Minute Medicine Rewind December 25, 2016
Dry Care Versus Antiseptics for Umbilical Cord Care: A Cluster Randomized Trial
Because omphalitis is rare in developed countries, the benefit of antiseptic use in umbilical cord care have not been shown. The purpose of this study was to assess the noninferiority of dry care compared with antiseptics in France on neonatal omphalitis. This was a cluster-randomized, 2-period crossover trial in 6 French university maternity units which included 8698 infants born after 36 weeks. Two 4-month study periods were separated by a 3-month wash out period in this 2-period trial. In the control period, the standard antiseptic techniques were utilized in cord care while in the dry care period, the cord was cleansed with non-antiseptic soap and water and gently dried. The primary outcome of interest was neonatal omphalitis. Among the 8698 participants, omphalitis occurred in 3 of 4293 (0.07%) newborns in the dry care group and in none of the 4404 newborns in the antiseptic care group (95% CI: -0.03 to 0.21). Other factors such as neonatal infection, parental appreciation of difficulty in care, and time to separation of the cord were not significantly different between the 2 groups. As a result, the authors concluded that dry cord was non-inferior to the use of antiseptics in preventing omphalitis in full term newborns in developed countries.
Association of Perioperative Statin Use with Mortality and Morbidity After Major Noncardiac Surgery
Although statins play a role in reducing cardiovascular events, their use in reducing perioperative risk of complications or mortality is controversial. The purpose of this study was to evaluate associations of early perioperative statin exposure on 30-day mortality and complications in the veteran population undergoing non-cardiac surgery. This was a retrospective observational cohort study which included 180,478 veterans undergoing elective or emergent non-cardiac surgery from 2005-2010. The primary outcome of interest was all-cause 30-day mortality and secondary outcomes included cardiovascular and non-cardiovascular complications. Statistical analysis included propensity score to match patients with statin exposure and no exposure as well as McNemar test and calculate relative risk ratios to compare the risk of outcomes between groups. A total of 94,486 were included in the propensity score-matched cohort (96.3% men; 3.7% women; mean [SD] age, 65.9 [10.6] years). 37.8% of patients had active outpatient prescription for statin. Exposure to a statin on the day of or the day after surgery was noted in 31.5% of the cohort. Among the 48,243 propensity-score matched pairs, 30-day all cause mortality was significantly reduced in statin exposed patients (RR 0.82; 95% CI: 0.75 to 0.89; p < 0.001). The number needed to treat was 244 (95% CI: 170 to 432). There was also a significant reduction in risk of any perioperative complication (RR 0.82; 95% CI: 0.79 to 0.86; p < 0.001). The number needed to treat was 67 (95% CI: 55 to 87). Greatest risk reduction was seen for cardiac complications (RR 0.73; 95% CI: 0.64 to 0.83). As a result, the authors concluded that early perioperative exposure to statin was associated with a significant decrease in all-cause perioperative mortality in the veteran population.
Survivorship in Children and Young Adults with Congenital Heart Disease in Sweden
Advancement in pediatric care has decreased the mortality in patients with congenital heart disease (CHD) however, there is limited data on survival trends in children and young adults with CHD compared to the general population. The purpose of this study was to determine the survivorship in children and young adults with CHD compared with matched controls. This registry-based prospective cohort study identified 21,982 patients with CHD born between 1970 and 1993 in Sweden. The main outcome of interest was the survivorship in young patients with CHD and controls. Of the 21,982 patients with CHD, 10,650 (48.4%) were female and the median age was 4.22 years. The survivorship among children younger than 5 years increased from 96% from those born in 1970-1979 to 98% in those born in 1990-1993 (hazard ratio (HR) for mortality compared to matched controls 225.84, 95% CI:136.84 to 372.70; to 33.47, 95% CI: 22.54 to 49.70). For young adults, the HRs for mortality did not significantly decrease over time: 1970 to 1979 (HR 7.79; 95%CI: 6.72 to 8.96),1980-1989 (HR 4.91; 95%CI: 3.99 to 6.02), and 1990-1993 (HR 4.26 95%CI: 2.29 to 7.94). For individuals with CHD, the mortality was higher compared to controls (HR 16.51, 95%CI: 15.29 to 17.83; p < 0.001). The authors concluded that despite increasing absolute and relative survivorship in children and young adults with CHD, the mortality remains high compared to those of matched controls.
Insurance Expansion and Hospital Emergency Department Access: Evidence from the Affordable Care Act
With the affordable care act (ACA), 8 million previously uninsured people obtained health insurance, however there is still not much known about how Medicaid expansion to households making below 138% of the federal poverty level has affected emergency department (ED) use. The purpose of this study was to determine how Medicaid expansion has affected ED use in terms of insurance status, visit type, and location. This was a quasi-experimental observational study which utilized a 2-group interrupted time-series model for Medicaid expansion and nonexpansion states from 2012-2014 with data utilized from two large hospital chains. The patients were uninsured and Medicaid-insured adults from 18-64 years of age. A sample of 8,929,881 patient visits were used with 1,057,818 of these visits coming from patients who lived in expansion states. The authors found that after one year of ACA implementation, Medicaid expansion state EDs saw a decrease of 47.1% (95% CI: -65% to -29.3%) in uninsured visits and an increase in 125.7% (95%CI: 89.2% to 162.6%) in Medicaid visits compared to a decrease of 5.3% (CI: −24.0 to 13.6) and an increase of 11.4% (95% CI: −43.6% to 51.3%), respectively, in nonexpansion states. Medicaid expansion state EDs also saw a decrease of −41.9% (95% CI: −53.1% to −30.8%) in uninsured visits and an increase of 212.9% (95% CI: 164.9% to 261.6%) in Medicaid visits compared to an increase of 0.8% (95% CI: −11.2% to 12.8%) and an increase of 15.7% (95% CI: −59.9% to 69.4%), respectively, in nonexpansion states for nondiscretionary conditions requiring immediate medical treatment. These changes suggest that Medicaid expansion resulted in significant changes in ED visits where found in terms of insurance status, visit types, and location in Medicaid expansion states compared to nonexpansion states.
During storage, red blood cells (RBCs) undergo physiological changes that may or may not be clinically significant and affect patient outcomes. Some prior studies suggest that the duration of RBC storage is associated with adverse patient outcomes including mortality while other studies find no association. This is a retrospective cohort study with patients selected from the Scandinavian Donations and Transfusions database. A total of 854,862 patients met the inclusion criteria and a cox regression analysis was performed of 30-day and 1-year mortality and the authors compared patients who received RBC units stored for different durations (0-9d, 10-19d, 20-29d, and 30-42d). No association was found between RBC storage and risk of death. Specifically, with 30 days and 1 year of follow up, the HR of death in recipients of units stored for 30-42 days was 0.99 (95% CI: 0.95 to 1.02) and 1.00 (95% CI: 0.98 to 1.02) respectively, compared to recipients of units stored for 10 to 19 days. Thus the authors concluded that there was no significant difference in mortality when comparing patients that received fresh versus stored blood and that the current practice of storing RBCs for up to 42 days does not need to be changed.
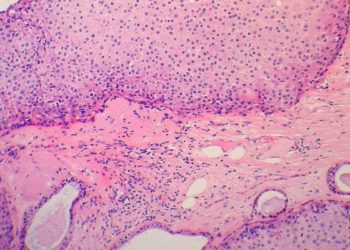
Image: PD
©2016 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.