2 Minute Medicine Rewind May 5, 2025
Maternal Hypertension and Adverse Neurodevelopment in a Cohort of Preterm Infants
1. Maternal hypertensive disorders of pregnancy (HDP) was independently associated with adverse cognitive and language outcomes at 2 years’ corrected age.
2. Brain abnormalities at term-equivalent age partially mediated 24% of the total effect of HDP on lower cognitive scores.
Evidence Rating Level: 2 (Good)
Hypertensive disorders of pregnancy (HDP) include preeclampsia, gestational hypertension, and chronic hypertension existing before pregnancy. Although exposure to HDP has been linked to suboptimal neurodevelopmental outcomes in full term-born children, findings in preterm infants remain conflicting. This study thus examined the association between maternal HDP and neurodevelopment in preterm infants born at 32 weeks or less. The prospective cohort study included 395 preterm infants (≤32 weeks’ gestation) from Cincinnati Infant Neurodevelopment Early Prediction Study (CINEPS), a multisite prospective regional cohort that recruited from five Ohio neonatal intensive care units from September 2016 to November 2019. HDP was defined by maternal diagnosis of chronic or gestational hypertension or preeclampsia during pregnancy. Brain magnetic resonance imaging (MRI) was performed at term-equivalent age. Global brain abnormality score (GBAS) was used to assess preterm brain injury and disrupted brain development. Neurodevelopment was assessed by Bayley Scales of Infant and Toddler Development (BSID), Third Edition, between 22 and 26 months’ corrected age. Of the 395 infants included in the study (median [interquartile range, IQR] gestational age = 29.6 [27.6-31.4] weeks, median [IQR] birth weight = 1,230 [950-1,628] g, male [%] =210 [53.2%]), 170 (43%) were exposed to HD, and 104 of 170 (61%) were exposed to preeclampsia. In total, 341 children (87%) completed the BSID. In adjusted analyses, HDP exposure was associated with lower BSID cognitive scores (β estimate = −3.69; 95% CI, −6.69 to −0.68; P = .02) and lower language scores (β estimate = −4.07; 95% CI, −8.03 to −0.11; P = .04). Preeclampsia exposure showed similarly negative but greater associations for BSID cognitive scores (β estimate = −4.85; 95% CI, −8.63 to −1.07; P = .01) and language scores (β estimate = −6.30; 95% CI, −11.49 to −1.09; P = .02). Brain abnormalities at term-equivalent age partially mediated 24% of the total effect of HDP on lower cognitive scores (β estimate = −0.82; 95% CI, −1.72 to −0.13; P = .02). Overall, this study found that maternal HDP was independently associated with adverse cognitive and language outcomes at 2 years’ corrected age, with greater effects in preeclampsia-exposed preterm infants. These findings highlight the importance of recognizing HDP as a risk factor for adverse neurodevelopmental outcomes, underscoring the need for early identification and targeted interventions to mitigate its impact.
Baseline lung function and risk of incident tuberculosis: a nationwide population-based cohort study
1. The risk of tuberculosis (TB) was higher in individuals with obstructive or restrictive lung function impairment compared to those with normal lung function.
2. TB incidence was inversely correlated with forced expiratory volume in 1 second.
Evidence Rating Level: 2 (Good)
Tuberculosis (TB) is a leading infectious disease, ranking among the top 10 causes of death globally. While it is known that lung function decreases after pulmonary TB infection, the association between baseline lung function and risk of incident TB is unclear. This study thus investigated the relationship between baseline lung function and TB development among the general population. This nationwide population-based cohort study used data from the Korea National Health and Nutrition Examination Survey (NHIS) between 2010 and 2016 and included 16,594 participants aged >40 years with spirometry results and no history of TB. Spirometry measurements included forced expiratory volume in 1 second (FEV1), forced vital capacity (FVC), and the FEV1/FVC ratio. Spirometry outcomes were categorized into three groups based on predicted normal values: normal (FEV1/FVC ratio≥0.7 and FVC≥80% of predicted), restrictive (FEV1/FVC ratio≥0.7 and FVC<80% of predicted), and obstructive lung function (FEV1/FVC ratio<0.7). Among the 16,457 participants included in the study, 12,666 (77.0%) had normal lung function (mean age [SD] = 56.19 [9.97] years, female [%] = 7,796 [61.55%]), 1,587 (9.6%) had restrictive pattern (mean age [SD] = 61.18 [10.3], female [%] = 828 [52.17%]), and 2,204 (13.4%) had obstructive pattern (mean age [SD] = 65.97 [9.36], female [%] = 576 [26.13%]). During a median follow-up period of 5.5 years (interquartile range 3.5–7.5), 72 were newly diagnosed with TB. Compared to participants with normal lung function, TB risk was higher in participants with obstructive lung function impairment (adjusted hazard ratio (aHR): 2.03, 95% CI: 1.12–3.68) and restrictive lung function impairment (aHR: 2.19, 95% CI: 1.120–4.29). Low FEV1 was associated with increased TB risk (aHR [lowest quartile vs. highest quartile]: 1.91, 95% CI: 1.05–3.50; aHR [lowest decile vs. highest decile]: 2.76, 95% CI: 1.14–6.70; both p for trends<0.0001). Overall, this study found that individuals with lower lung function had an increased risk of TB, which may be inversely correlated with FEV1. Future prospective studies are needed to explore the mechanisms behind these findings.
1. The Endothelial Activation and Stress Index (EASIX) is associated with in-hospital, short-term (28-day), and long-term (365-day) all-cause mortality in critically ill patients with atrial fibrillation (AF).
2. EASIX is a reliable indicator of poor prognosis in critically ill patients with AF.
Evidence Rating Level: 2 (Good)
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia and is strongly linked to increased risks of all-cause mortality, heart failure, hospitalization, and thromboembolic events. Many studies have shown an association between endothelial dysfunction (ED) and the development and progression of AF. The Endothelial Activation and Stress Index (EASIX) is a novel biomarker for assessing endothelial health and has been validated as a prognostic marker for mortality in various health conditions. However, research on the role of EASIX as a prognostic marker in patients with AF is limited. This study thus assessed the association between EASIX and prognosis in critically ill patients with AF. This retrospective study analyzed data from the Medical Information Mart for Intensive Care IV(MIMIC-IV) database and included patients aged 18-99 years with AF who had an intensive care unit stay of more than 24 hours. EASIX was calculated using the formula: lactate dehydrogenase (U/L) × creatinine (mg/dL)/platelets (109 cells/L) and log2-transformed for statistical analysis. Patients were grouped by EASIX quartiles: Q1: < 4.56, Q2: 4.56–5.64, Q3: 5.64–6.84, and Q4: > 6.84. In total, 4,896 patients were included (median age [interquartile range] = 75 [66, 83] years, male [%] = 2,871[58.64%]). All-cause mortality rates for in-hospital, 28-day, and 365-day were 26.04%, 29.25%, and 49.75%, respectively. Higher EASIX was associated with increased in-hospital (OR 1.28, 95% confidence interval [CI] 1.19–1.37), 28-day (HR 1.21, 95% CI 1.16–1.26, P < 0.001), and 365-day HR 1.16, 95% CI 1.12–1.21) all-cause mortality after multivariable adjustment. For each time point, patients in quartiles Q2, Q3, and Q4 had significantly higher mortality than those in Q1. The performance of EASIX in predicting both 28-day and 365-day all-cause mortality was comparable to the Sequential Organ Failure Assessment (SOFA) and higher than the CHA₂DS₂–VASc score. Overall, this study found that EASIX is associated with in-hospital, short-term, and long-term all-cause mortality in critically ill patients with AF and that EASIX is a reliable indicator of poor prognosis in this patient population. Future prospective studies are necessary to confirm study findings.
Menstrual Cycle Length Changes Following Vaccination Against Influenza Alone or With COVID-19
1. Influenza vaccine given alone or concurrently with a COVID-19 vaccine was associated with a small (< 1 day) but temporary change in menstrual cycle length.
Evidence Rating Level: 2 (Good)
Previous studies have reported menstrual disturbances following COVID-19 vaccination, including temporary changes in menstrual cycle length and heaviness in menstrual flow. As menstrual health outcomes have been largely overlooked in previous vaccine clinical trials, research on vaccine-related menstrual changes is limited, particularly for the influenza vaccine and its co-administration with the COVID-19 vaccine. This study thus examined whether influenza vaccination alone or combined with COVID-19 vaccination is associated with changes in menstrual cycle length. This global retrospective cohort study used prospectively collected menstrual cycle data from a digital birth control application from April 25, 2023, to February 27, 2024 (4-5 cycles per individual). Participants aged 18 to 45 years were included if they were not using hormonal contraception and had average cycle lengths of 24 to 38 days across three consecutive cycles prior to vaccination. Among the 1,501 individuals included in the study, 791 were vaccinated for influenza only and 710 were concurrently vaccinated for influenza and COVID-19. Most participants were younger than 35 years (1,230 [82%]). Individuals vaccinated for influenza alone experienced an adjusted mean increase of 0.40 (95% CI, 0.08-0.72) days in menstrual cycle length, while those vaccinated concurrently for influenza and COVID-19 experienced a mean increase of 0.49 (95% CI, 0.16-0.83) days (P = .69 for difference between vaccine groups). During the vaccination cycle, a slightly higher percentage of individuals who received both vaccines concurrently experienced a clinically meaningful change in cycle length of >8 days compared to those who received only the influenza vaccine (42 of 710 [5.9%] vs 37 of 791 [4.7%]), although the difference was not statistically significant. Both vaccination groups returned to their prevaccination cycle lengths in the postvaccination cycle. Menstrual cycle changes were identified when vaccination occurred in the follicular phase, with an increase of 0.82 [95% CI, 0.40-1.24] days for influenza alone and 0.99 [95% CI, 0.55-1.43] days for concurrent influenza and COVID-19 vaccine, but not the luteal phase. Overall, this study found that receiving influenza concurrently with COVID-19 vaccines was associated with a small but temporary change in menstrual cycle length. These findings may assist clinicians in reassuring patients who are concerned about potential menstrual side effects of vaccination.
1. In this population-based cohort study, patients with varicose veins (VV) had an increased risk of all-cause dementia.
2. Treatment of VV was associated with a reduced risk of vascular dementia.
Evidence Rating Level: 2 (Good)
Varicose veins (VV) are characterized by enlarged and twisted superficial veins that are >3mm in diameter, primarily affecting the saphenous veins, their branches, or other superficial veins in the legs. Previous research has linked VV to white matter changes in the brain, increased inflammation, and endothelial dysfunction, which may trigger neuroinflammatory pathways associated with dementia and vascular cognitive impairment. Although VV and dementia are both prevalent, the potential link between them remains unclear. This study thus investigated the relationship between VV and dementia risk, as well as whether treatment or procedures for VV are associated with dementia risk. This retrospective study analyzed data from the National Health Insurance Service-Health Screening (NHIS-HEALS) cohort database in South Korea and included participants aged >40 years who had available health screening results between 2005 and 2010. In total 396,767participants were included in the study (mean age [SD] = 56.1 [9.3], male [%] = 182,347 [46.0%]), with VV present in 5,096 (1.3%) participants. During a median follow-up of 13.33 years (interquartile range 10.4–16.26), 55,329 (13.9%) cases of all-cause dementia were identified. Compared to the non-VV group, the VV group had an increased risk of all-cause dementia (hazard ratio [HR]: 1.235, 95% confidence interval [CI]: 1.147–1.329). Treatment or procedures for VV was significantly associated with a decreased risk of vascular dementia (HR: 0.566, 95% CI: 0.382–0.841). Overall, this study found that patients with VV had an increased risk of all-cause dementia, while treatment of VV was associated with a reduced risk of vascular dementia.
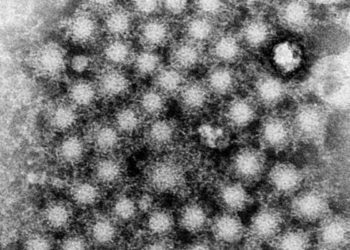
Image: PD
©2025 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.