2 Minute Medicine Rewind November 24, 2025
1. Incidence rates of hypertension and opportunistic and serious infections increase with age in patients receiving ozanimod for ulcerative colitis (UC).
Evidence Rating Level: 1 (Excellent)
Treating older patients with UC is difficult due to an overreliance on corticosteroids and hesitancy in using more advanced therapies due to the increased risk of adverse events such as infection, major adverse cardiovascular events, thromboembolic complications, and malignancies. Ozanimod is a selective sphingosine 1-phosphate (S1P) receptor 1 and 5 modulator approved for the treatment of moderately to severely active UC. This article uses data from the True North study, a randomized, placebo-controlled phase 3 trial. In the 10-week induction period, patients in cohort 1 were assigned to receive ozanimod 0.92 mg or placebo, and patients in cohort 2 received open-label ozanimod at the same daily dose. At 10 weeks, patients with a clinical response to ozanimod in either cohort underwent randomization again to receive double-blind ozanimod or placebo for the maintenance period (through week 52). 1012 total patients were stratified by age: < 40 (n = 492; mean [range] age: 30.0 [18-39]; 56.3% male), 40-60 ((n = 404; mean [range] age: 49.4 [40-60]; 64.4% male), and > 60 (n = 116; mean [range] age: 65.2 [61-74]; 56.0%). Rates of treatment-emergent adverse events (TEAEs) were higher in patients receiving continuous ozanimod (47.7%-53.6%) than in those who switched to placebo (34.3%-39.2%) in all age groups. Exposure-adjusted incidence rates (EAIRs) of opportunistic infection (eg, herpes zoster), COVID-19, and serious infection increased with age. Patients ≥ 40 years of age had higher hypertension EAIRs than those < 40 years of age. These results suggest a need for greater monitoring of side effects in older patients receiving ozanimod for IBD. This may include herpes zoster vaccinations and increased monitoring of cardiac adverse reactions.
1. Low bicarbonate replacement fluid (LBF) leads to more stable pH and HCO3− compared to high bicarbonate replacement fluid (LBF) during continuous veno-venous hemofiltration with regional citrate anticoagulation (RCA).
Evidence Rating Level: 1 (Excellent)
CVVH with RCA causes alkalinization due to the metabolic conversion of citrate to carbonate. Thus, the bicarbonate concentration of the CVVH replacement fluid is a key determinant of systemic pH. However, very few protocols have been published on acid-base changes in CVVH. This prospective, randomized, controlled, cross-over trial randomized 88 patients to receive either LBF (22 mmol/l HCO3−, median [IQR] age, 64.5 [54.5-70.5]; 73% male) or HBF (30 mmol/l HCO3−, median [IQR] age, 64.5 [60.5-73.0]; 64% male) for 48 hours, after which the replacement fluid was switched and treatment was continued for another 48 hours after a 3 hour washout period. The primary endpoint was incidence of pH or HCO3− excursion, defined as pH > 7.45 or HCO3− > 26 mmol/l within 16–48 h of each treatment phase. Patients in the HBF group had a significantly higher incidence of pH (OR 1.78, 95% CI 1.12–2.82; p = 0.015) and HCO3− (OR 3.60, 95% CI 2.16–5.99; p < 0.001) excursions. There was no significant difference in the time to pH (p = 0.102) or HCO3− normalization (p = 0.468). In summary, this study found LBF during CVVH with CRA leads to a more stable acid-base profile in terms of pH and HCO3− compared to HBF. Future research is needed to determine if this translates to improved long-term outcomes.
Age-Based Screening for Lung Cancer Surveillance in the US
1. Current US Preventive Services Task Force (USPSTF) screening criteria for lung cancer excludes many at-risk individuals and has poor adherence – age-based screening is cost-effective and improves detection.
Evidence Rating Level: 2 (Good)
Current USPSTF guidelines for lung cancer screening includes patients aged 50-80 years, have ≥ 20 pack-years, and are currently smoking or or quit < 15 years ago. Low-dose computed tomography (LDCT) has been proven to be effective for early detection; however, participation rates remain below 15% of eligible individuals, and there exist multiple nontobacco risk factors in lung cancer development. The authors sought to determine what proportion of patients meet USPSTF criteria, and if age-based screening would improve detection and be cost-effective. This retrospective cohort study found that of 997 patients (median [IQR] age: 67 [18-99]; 58.0% female) diagnosed with lung cancer, 45 patients underwent LDCT screening. 35.1% met USPSTF screening criteria, and 12.6% of these patients underwent LDCT screening. Expanding criteria to age 40 to 85 years, 10 or more pack-years, and no cessation limit increased detection to 62.1% (619 of 997 patients). Age-based screening (40-85 years) captured 93.9% of cases and prevented 26,124 deaths annually (95% CI, 20,000-32,248 deaths annually) at $101,000 per life saved (95% CI, $82,000-$120,000). This study suggests current USPSTF guidelines have poor adherence and are insufficient at capturing the majority of patients with lung cancer. Age-based screening improves detection and is cost-effective.
Prehospital Postintubation Hypotension and Survival in Severe Traumatic Brain Injury
1. Prehospital postintubation hypotension after traumatic brain injury (TBI) is common and associated with a significantly increased incidence of mortality.
Evidence Rating Level: 2 (Good)
Preventing systemic insults from hypotension, hypoxia, and hypocapnia is key to improving outcomes after TBI. However, a substantial proportion of patients with TBI require prehospital rapid sequence intubation, which can cause postintubation hypotension. This retrospective, multicenter, observational cohort study measured the association between postintubation hypotension (systolic blood pressure (SBP) <90 mmHg at 10 minutes or less of induction) and 30-day mortality for patients with severe TBI (head Abbreviated Injury Score (AIS) ≥ 3). Of 1539 patients (median [IQR] age: 48[29-66]; 73.5% male), 19.1% had postintubation hypotension. Postintubation hypotension was significantly associated with increased 30-day mortality (AOR, 1.70; 95% CI, 1.01-2.86; P = 0.04). Furthermore, statistically significant differences in mortality were observed for postintubation SBP up to 100 mmHg. This observation remained when looking at patients with isolated severe TBI (head AIS score ≥3 and all other body region AIS scores <3) who had postintubation hypotension (AOR, 13.55; 95% CI, 3.65-61.66; P < 0.001). These findings suggest postintubation hypotension is common and associated with increased mortality. Further studies should assess ways to reduce the incidence of postintubation hypotension in the prehospital setting when advanced airway management is required.
1. The novel SAVE risk score is effective at identifying non-ST-segment elevation acute coronary syndrome (NSTE-ACS) patients with totally occluded infarct-related artery (IRA-TOCA), potentially guiding timely percutaneous coronary intervention (PCI).
Evidence Rating Level: 2 (Good)
Current NSTE-ACS management guidelines recommend antiplatelet and anticoagulation therapy. However, even in NSTE-ACS patients, coronary angiography reveals 30% of patients have IRA-TOCA. Early invasive strategies such as PCI are reserved for high-risk NSTE-ACS patients, commonly determined using the Global Registry of Acute Coronary Events (GRACE) score. This study sought to validate the novel SAVE score, which combines clinical, ECG, and echocardiographic findings. 185 NSTE-ACS patients were categorized into IRA-TOCA (n = 61; mean [SD] age: 61.6 [10.1]; 82.0% male) and IRA-NTOCA (n = 124; mean [SD] age: 61.5 [10.3]; 79.0% male). The GRACE score was not able to differentiate between IRA-TOCA and IRA-NTOCA (p = 0.384). The SAVE score demonstrated a significantly higher proportion of high-risk patients (score ≥3) in the IRA-TOCA group (73.8% vs. 45.2%; P < 0.001), with a sensitivity of 73.77% and a specificity of 54.84% for demonstrated NSTE-ACS patients with IRA-TOCA. These findings suggest the SAVE score may be more effective than the commonly used GRACE score at identifying NSTE-ACS patients with IRA-TOCA requiring early PCI. Prospective studies are required to validate these findings.
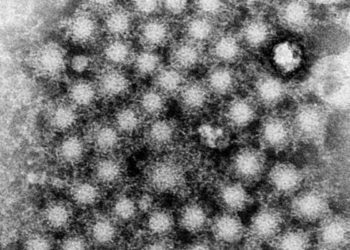
Image: PD
©2025 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.