4PEPS clinical probability score may reduce need for imaging in suspected pulmonary embolism
1. The 4PEPs strategy (4-Level Pulmonary Embolism Clinical Probability Score) may be a useful tool for emergency department physicians in patients suspected of pulmonary embolism.
2. Applying 4PEPs reduced the need for imaging testing and showed false-negative testing rates below 1%.
Evidence Rating Level: 2 (Good)
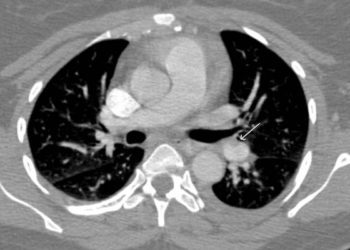
Study Rundown: This study investigated whether using a pretest probability score could safely reduce the need for image testing, namely computed tomography pulmonary angiography, or CTPAs, by using clinical criteria and optimized D-dimer measurements to rule out pulmonary embolisms (PE). While using D-dimer testing with CTPA is the standard diagnostic strategy, there has been a large influx in CTPA testing for suspected PE. Due to the lack of specificity of D-dimer testing and the common symptoms of a PE, more CTPAs have been used to rule out false positives. Although CTPAs are accessible, fast, minimally invasive, and more sensitive than ventilation/perfusion scans, they may unnecessarily expose patients to risks of allergies, kidney failure, and cumulative radiation-induced cancer.
By integrating all proposed diagnostic scoring strategies into the 4-Level Pulmonary Embolism Clinical Probability Score (4PEPS) and combining patients suspected of PE from 5 multicentre cohorts, this study developed and validated a scoring system that could help physicians safely and effectively decrease image testing for PEs. Applying the 4PEPS resulted in <1% false-negative test rates and out-performed all previous proposed diagnostic strategies for PE, which suffered from issues with reliability or inaccuracy in populations with higher PE prevalence when used independently. However, some potentially relevant criteria (ie pregnancy, history of cancer, hemoptysis) were not found to be statistically associated with a PE diagnosis, more likely due to the lower threshold physicians use when PE is suspected in these populations than due to a lack of power in the study. In fact, the multiple databases used allowed for cohorts with large populations, which were also very similar to each other (AUC 80%). Established guideline recommendations were followed to derive and validate their 4PEPs strategy and they used a bayesian approach to define prevalence limits per CPP category. Nonetheless, considering the cohorts used, 4PEPs may not be applicable to patients outside the ED settings (ie inpatients) and certain variables could not be systematically collected and thus could not be included in analyses. Finally, a 13-variable score may be difficult to memorize, suggesting the need for its calculation on an electronic device. Ultimately, a prospective implementation study is necessary to formally validate 4PEPS as a tool to determine whether patients suspected of PE need imaging testing.
Click to read the study in JAMA Cardiology
Relevant Reading: Trends in Imaging for Suspected Pulmonary Embolism Across US Health Care Systems
In-Depth [retrospective cohort study]: This retrospective analysis gathered data from 11 114 patients, which were merged from three prospectively collected databases for derivation and internal validation, while two other databases were used for external validation. Four levels of CPP (clinical pretest probability) were outlined, from very low, which excludes PE only through clinical criteria, and high CPP, which necessitates imaging testing (CTPA or V/Q scan) and does not allow for the safe exclusion of PE by D-dimer testing. In deriving the score, 2% was the safety threshold for PE and in each CPP category, the upper limit for PE prevalence was predefined using the Bayesian approach. 4PEPS was created through the evaluation of all clinical variables associated with suspicion of PE, but removed any variables where more than 2% of data was missing (ie history of hypertension, long travel, body weight, respiratory rate, antiplatelet treatment), with the exception of variables included in other prediction rules (ie PERC strategy, revised Geneva score, Wells score). In the derivation cohort of 55 888 patients (61.8% female, mean age 52 years), PE prevalence 11.0%, compared to 11.7% in the internal validation cohort (3 726 patients), 21.5% in the first external validation cohort (1 548 patients), and 11.7% in the second external validation cohort. (1 669 patients). According to a univariate analysis, 21 variables were significantly associated with PE diagnosis; these 21 variables in addition to “estrogenic treatment”, were included in the multivariate models. 13 final variables which were significantly associated with PE diagnosis were included in the final model from which 4PEPS was derived and given points according to their regression coefficient: these include age <50 or 50-64 (-2), 50-64 (-1), chronic respiratory disease (-1), heart rate <80 beats per minute (-1), chest pain and acute dyspnea (+1), male (+2), hormonal estrogenic treatment (+2), personal history of VTE (+2), syncope (+2), immobility within the last 4 weeks (+2), pulse oxygen saturation <95% (+3), calf pain and/or unilateral lower limb edema (+3), and PE is the most likely diagnosis (+5). Clinical probability was separated into 4 categories, with a score of <0 allowing PE to be ruled out at very low CPP (<2%), while high CPP (>65%) from a score > 13 suggested PE could not be ruled out without imaging testing. The accuracy of the score was assessed through analyzing the area under the receiver operating characteristic curve (AUC), which were 0.79 (95% CI 0.76-0.82) and 0.78 (95% CI 0.74-0.81) for the first and second external validation cohorts respectively. Were the 4PEPS strategy to be used, false negative testing rates were estimated at 0.71% (95% CI 0.37-1.23) and 0.89% (95% CI 0.53-1.49) in the first and second external validation cohorts, with -22% (95% CI -26 to -19) and -19% (95% CI -22 to -16) reductions in imaging testing respectively.
Image: PD
©2020 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.