Amyloid-beta (1-40) is a strong predictor of mortality in acute coronary syndrome
1. Patients with the highest Aβ40 also had the worst non-ST-segment elevation acute coronary syndrome (NSTE-ACS) risk profile.
2. Greater all-cause mortality was observed in patients with higher circulating Aβ40.
Evidence Rating Level: 2 (Good)
Study Rundown: Acute coronary syndrome (ACS) remains a major cause of morbidity and mortality. Identifying predictors and risk stratification for patients NSTE-ACS is critical in order to identify patients in need of early coronary intervention and medication optimization. The authors of this study aimed to evaluate Amyloid-Beta (1-40) (Aβ40) in terms of its prognostic value regarding adverse outcomes in stable coronary artery disease. Aβ40 is pro-inflammatory and pro-thrombotic and is thought to play a role in coronary disease. Specifically, it is involved in the physiologic process related to plaque destabilization; therefore, it may reflect risk of adverse events regarding ACS. In general, it was found that circulating Aβ40 could be used as a predictor of mortality and improves risk stratification of patients with NSTE-ACS. The limitations of the study include the retrospective design and the fact that the endpoints did not incorporate individual cardiovascular outcomes. Rather, the study utilized all-cause mortality and new MI as endpoints.
Click to read the study in Annals of Internal Medicine
Relevant Reading: Novel Risk Markers and Risk Assessments
In-Depth [retrospective cohort]: The authors conducted a retrospective cohort study utilizing academic hospitals in seven European countries from 2 independent prospective cohorts, the Heidelberg study (n = 1145) and the validation multicenter international APACE (n = 734). The primary end point was all-cause mortality, while the secondary end-points included composite of death or nonfatal acute MI after a median follow-up of 21.9 months.
Research protocol did not interfere with patient management throughout the study. Generally, it was found that higher circulating Aβ40 was also associated with higher all-cause mortality after multivariate adjustment for age, sex, diabetes mellitus, and high-sensitivity cardiac troponin T and C-reactive protein, among other factors. For example, the Heidelberg cohort hazard ratio [HR] for the 80th percentile for Aβ40 compared to the 20th percentile was 1.66 [95% CI, 1.06 to 2.61; P = 0.026]. Similarly, for the APACE cohort the HR was 1.50 [CI, 1/15 to 1.96; P = 0.003]. As well, it was determined that the Aβ40 accurately reclassified risk for death over the Global Registry of Acute Coronary Events (GRACE) score—a score that is widely recommended for risk stratification in patients with stable coronary artery disease.
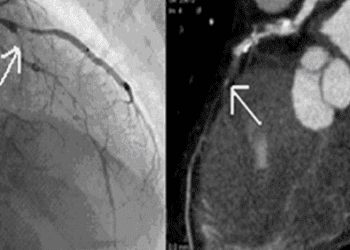
Image: PD
©2018 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.