Cervical medial branch blocks may offer therapeutic benefit for facet-mediated neck pain
1. A subset of patients undergoing cervical medial branch blocks experienced meaningful short- to medium-term pain and functional improvement that exceeded the expected duration of local anesthetic effects.
Evidence Rating Level: 2 (Good)
Study Rundown: This prospective cohort study by Finlayson et al. evaluated whether cervical medial branch blocks (CMBB), typically used diagnostically for facet-mediated neck pain, offer therapeutic benefit beyond the expected anesthetic duration. Among 179 patients (average age 58, mostly female) with prior ≥50% pain relief from CMBB, ultrasound-guided lidocaine injections were administered across 830 cervical levels. Patients were followed for 12 weeks, assessing pain (Numerical Rating Scale), disability (Neck Disability Index), emotional health (PHQ-9, GAD-7, PCS), and global impression of change (PGIC). At two weeks, 62.2% achieved ≥30% pain reduction, but this declined to 22.7% at 12 weeks, with similar patterns in functional and emotional outcomes. Exploratory analysis found no significant associations between demographic factors or clinical variables and pain relief durability. While benefits diminished over time, the findings suggest CMBB may offer modest short- to medium-term therapeutic effects, supporting further research on repeated use and patient selection for extended relief.
Click to read the study in Regional Anesthesia & Pain Medicine
Relevant Reading: Cervical zygapophyseal joint pain patterns. I: A study in normal volunteers.
In-Depth [prospective cohort study]: Facet joint pain is implicated in up to 40% of cases of axial neck pain, while cervicogenic headaches account for about 20% of chronic headaches, making these conditions common and challenging clinical problems. CMBB is typically used to identify patients who may benefit from more definitive treatments, such as radiofrequency ablation, by providing short-term pain relief lasting only as long as the local anesthetic (usually a few hours). However, prior reports and anecdotal observations have suggested that some patients experience prolonged pain relief after CMBB, sometimes lasting weeks or even months, though the mechanisms behind this extended benefit remain unclear. To address the frequency, magnitude, and duration of such therapeutic effects in routine clinical practice, the authors conducted a prospective observational study of 179 patients (average age 58, 80% female, primarily with degenerative joint disease) who had previously reported at least 50% pain relief from CMBB. In total, 830 cervical levels were treated using ultrasound-guided injections of lidocaine, performed in an outpatient setting by experienced practitioners. Patients were monitored over a 12-week period with structured online questionnaires assessing average weekly pain (Numerical Rating Scale, NRS), functional disability (Neck Disability Index, NDI), emotional well-being (Patient Health Questionnaire-9, PHQ-9; Generalized Anxiety Disorder-7, GAD-7; Pain Catastrophizing Scale, PCS), and overall patient perception of change (Patient Global Impression of Change, PGIC). Key inclusion criteria were prior successful CMBB response, chronic neck pain for at least four months, a baseline pain score of at least 5/10, and no active radicular symptoms; patients on anticoagulants or with certain comorbidities were excluded. The statistical approach used growth curve modeling to assess changes over time, with corrections for multiple comparisons. The study found statistically and clinically significant improvements at both the 2-week and 12-week time points compared to baseline. At 2 weeks, 62.2% of patients achieved at least a 30% reduction in pain scores, and 44.6% reported at least 50% pain relief. These benefits, however, diminished over time: by 12 weeks, only 22.7% maintained a 30% reduction, and just 13% continued to experience 50% relief. Similarly, functional improvements (as measured by NDI) and emotional health gains (PHQ-9, GAD-7, PCS scores) were most prominent at early follow-ups, tapering gradually by the end of the 12-week observation period. Interestingly, the exploratory analysis found no significant association between demographic or clinical factors — including age, opioid use, pain etiology, prior surgery, or the specific cervical levels treated — and the degree or persistence of pain relief. Notably, higher baseline depressive symptoms correlated with higher baseline pain and a more rapid return of symptoms after the initial improvement. The authors contextualize their findings by comparing them to prior studies, which have shown mixed results, possibly influenced by differences in anesthetic agents, adjunctive steroid use, and study designs. While radiofrequency ablation remains the standard intervention for patients who achieve diagnostic block success and seek longer-term relief, this study suggests that a subset of patients may derive meaningful short- to medium-term benefit from CMBB alone. The potential therapeutic role of repeat CMBBs, spaced at regular intervals, is intriguing, particularly for patients seeking alternatives to neuroablative procedures or for those not eligible for them. The authors note that possible mechanisms for the extended benefit include not just nociceptive blockade but also anti-inflammatory effects, modulation of central sensitization, and psychosocial factors such as improved mood following temporary pain reduction.
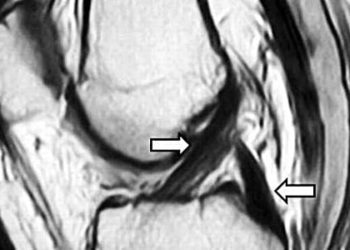
Image: PD
©2025 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.