Device thrombosis more likely with bioresorbable scaffolds versus drug-eluting stents
1. Device thrombosis occurred at a higher rate in patients undergoing percutaneous coronary intervention (PCI) utilizing a bioabsorbable scaffold compared to a metallic stent, both of which were covered in everolimus.
2. Failure of vessel revascularization and cardiac death occurs at similar rates for PCI procedures utilizing bioresorbable scaffolds and metallic stents.
Evidence Rating: 1 (Excellent)
Study Rundown: Drug-eluting stents (DES) are commonly used in PCI for treating coronary artery disease (CAD), though their rigid intravascular structure is associated with a risk of reocclusion. A new type of device, bioresorbable scaffolds, could potentially improve vessel function without leaving a permanent intravascular structure prone to reocclusion. Prior work has been mixed regarding reocclusion rates of bioresorbable stents compared to DES. As bioresorbable scaffolds have become more widely approved, better comparison of devices utilized in routine clinical practice and with longer follow-up is needed.
This randomized study looked to compare rates of vessel reocclusion and complications of reocclusion for patients undergoing PCI using bioresorbable scaffolds and DES, both covered in the immunosuppressant everolimus. Patients included in the study had CAD deemed suitable for PCI. Comparing treatment groups at 2 years follow-up, no difference was observed between treatment groups regarding rates of target-vessel failure, revascularization, or cardiac death. Thrombosis was more likely in the bioresorbable scaffold group, as was target-vessel myocardial infarction (MI). This study suggests the pathologic process of thrombosis, and clinically significant target-vessel MI, may be more common in vessels treated with bioresorbable scaffolds. These results suggest further evaluation of bioresorbable scaffold efficacy is needed, even though rates of cardiac death and target-vessel failure occur at similar rates compared to DES.
Click to read the study, published in NEJM
Relevant Reading: Improving vessel healing with fully bioresorbable drug-eluting stents: more than a pipe dream?
In-Depth [randomized controlled trial]: This noninferiority, randomized clinical trial enrolled 1845 patients in the Netherlands between 2013 and 2015. Enrolled patients had CAD and vascular lesions amenable to PCI. Randomization distributed patients in a 1:1 manner into bioresorbable vascular scaffold (n = 924) and drug-eluting stent (n = 921) treatment groups, and both devices were coated with everolimus. During the first year following placement, 63% of patients in the scaffold group had redilation procedures performed. Both groups received antiplatelet therapy per guidelines. Patients were followed for up to 5 years after the procedure to assess primary endpoints of cardiac death, target-vessel MI, and target-vessel failure, and secondary endpoints of device thrombosis and total death, MI, or revascularization events. Mean follow-up was 707 days. Target-vessel failure occurred in 105 scaffold patients and 94 stent patients (HR with bioresorbable scaffolds 1.12; 95%CI 0.85-1.48; p = 0.43). Cardiac death at 2 years occurred in 18 (2.0%) scaffold and 23 (2.7%) stent patients, respectively (HR 0.78; 95%CI 0.42-1.44; p = 0.43). Target-vessel MI occurred in 5.5% of scaffold and 3.2% of stent patients, respectively (HR, 1.60; 95%CI 1.01-2.53; p = 0.04). Definite or probable device thrombosis occurred at 2 years in 3.5% of scaffold and 0.9% of stent patients, respectively (HR, 3.87; 95%CI 1.78-8.42; p < 0.001).
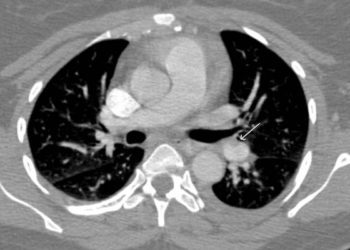
Image: PD
©2017 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.