ECMO for severe ARDS does not improve mortality
1. Extracorporeal membrane oxygenation (ECMO) for severe acute respiratory distress syndrome (ARDS) did not show a 60-day mortality benefit compared to conventional ventilation and ECMO rescue therapy.
2. There were more adverse events in the ECMO group with respect to bleeding requiring transfusion and severe thrombocytopenia.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Patients with ARDS have high mortality rates given current interventions, which includes low-volume, low-pressure ventilation strategies. Although ECMO has been used in cases of severe ARDS with encouraging results, limited conclusions could not be drawn from these experimental trials. As such, this randomized controlled trial aimed to compare the use of venovenous ECMO to conventional mechanical ventilation (which included ECMO rescue therapy) in patients with severe ARDS. The results showed no significant mortality benefit in the ECMO group at 60 days. Additionally, the frequency of complications did not differ significantly between the two groups, though increased bleeding and severe thrombocytopenia was observed in the ECMO group.
Strengths of this trial include it’s randomized, multi-center design evaluating patients with severe ARDS, where improved treatment would be expected to show substantial differences in outcomes. The trial does have limitations, of which it was stopped before the maximum calculated sample size was achieved, 28% of the control group received ECMO for refractory hypoxemia which may have diluted the ECMO effect, and patients were included from both specialist and non-specialist ECMO centers which may have led to differing levels of care.
Click to read the study, published in NEJM
Relevant Reading: Acute respiratory distress syndrome
In-Depth [randomized controlled trial]: This study aimed to demonstrate the efficacy of venovenous ECMO in patients with severe ARDS in reducing mortality. Patients were eligible if they met guidelines for severe ARDS and had undergone endotracheal intubation for less than 7 days. Notable exclusion criteria include patients intubated for longer than 7 days, a BMI of greater than 45, or significant pulmonary, cardiac, or malignant conditions. The trial allowed for crossover to ECMO for patients in the control group who had refractory hypoxemia. The primary endpoint was mortality at 60 days.
There were 1015 patients eligible for study inclusion, with 249 patients ultimately undergoing randomization: 124 were assigned to the ECMO group, and 125 were assigned to the control group. Of the 124 ECMO patients, 1 patient had rapid clinical improvement and 2 patients died soon after randomization. In the control group, 35 patients crossed over to the ECMO group due to refractory hypoxemia. At 60 days, 44 patients in the ECMO group and 57 patients in the control group had died (relative risk [RR], 0.76; 95% confidence interval [CI], 0.55 to 1.04; p = 0.09). The hazard ratio comparing the ECMO and control group was 0.70 (95% CI, 0.47 to 1.04; p = 0.07). There was one patient in each of the ECMO and control groups who died from complications related to the ECMO cannulation. Those in the ECMO group had higher rates of severe thrombocytopenia (27% vs 16%; absolute risk difference, 11%; 95% CI, 0 to 21%) and bleeding events requiring packed red-cell transfusion (46% vs 28%; 95% CI, 6 to 30%).
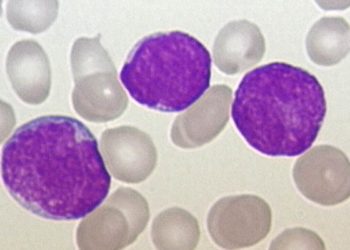
Image: PD
©2018 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.


![Reinnervation of cardiac infarcts decreases subsequent arrhythmia incidence [PreClinical]](https://www.2minutemedicine.com/wp-content/uploads/2015/02/1280px-Heart_ant_wall_infarction-350x250.jpg)