Government-funded initiatives provide important supports to low-income HIV patients
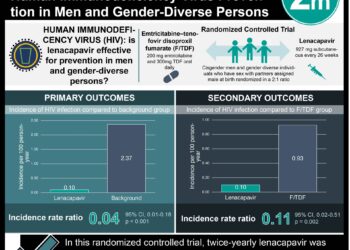
1. Almost 75% of HIV-infected adults in the USA received medical and support services from a Ryan-White HIV/AIDS funded facility.
2. Poorer patients were more likely to achieve viral suppression, receive case management and have access to substance abuse and mental health supports if they received care at a Ryan-White HIV/AIDS program.
Evidence Rating Level: 2 (Good)
Study Rundown: The Ryan-White HIV/AIDs program (RWHAP) was initiated in 1990 to help low-income, uninsured and underinsured individuals gain access to high-quality HIV care, treatment and supports. They provide access to outpatient medical care, HIV treatment medications, antiretroviral therapy adherence support, as well as non-medical assistance with food, housing, transportation, mental health services and risk reduction counseling. Since the initiation of the Patient Protection and Affordable Care Act, which will now expand health care coverage to HIV infected persons, it is important to understand the role that RWHAP plays in providing both medical but more importantly non-medical services to this underserved population. This study aimed to examine the differences between RWHAP and non-RWHAP-funded facilities with respects to services provided and patient outcomes.
Patients served by RWHAP facilities were more likely to be female, young, of non-Caucasian ethnic background, have less than high school education, low socioeconomic status and not have health coverage. At RWHAP facilities these patients were equally likely to have access to medical antiretroviral therapy. They also had increased access to case management, substance abuse and mental health services, adherence/risk counseling and other social services. Strengths of this study include providing insight into existing government-funded facilities which provide important services to patients of low socioeconomic status. Limitations of this study include having some missing information funding statuses for some facilities and also having a generally lower response rate (ranging from 76% to 83%).
Click to read the study, published today in JAMA Internal Medicine
Relevant Reading: Antiretroviral treatment of adult HIV infection: 2014 recommendations of the International Antiviral society
In-Depth [retrospective cohort]: This study used data from the Medical Monitoring Project cross-sectional study that included information on 8038 HIV-infected adults across the United States and was conducted from June 2009 to May 2012. This survey included information on patient and facility characteristics, and was used to compare the demographic/socioeconomic patient features, service needs and access to services at RWHAP-funded vs. non-RWHAP-funded facilities. In particular, differences in prescribed antiretrovirals and viral suppression were assessed.
Overall, 35% of facilities receive funding from RWHAP, and these facilities serve approximately 75% of the American HIV-infected population. Patients served at RWHAP facilities were younger, more often female, of African-American or Hispanic ethnicity, had low socioeconomic status, no health coverage and also had less than high school education. In addition to providing medical HIV treatment to their patients, the RWHAP facilities were more likely to provide case management (76.1% vs. 15.4%), and substance abuse (33.6% vs. 12.0%) or mental health services (64.0% vs. 18.0%). The degree to which patients received antiretroviral therapy was similar between RWHAP and non-RWHAP facilities. However, poorer patients were more likely to achieve viral suppression if they attended a RWHAP facility (adjusted prevalence ratio 1.09; 95%CI 1.02-1.16).
Image: PD
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.