HIV-positive-to-HIV-positive kidney transplantation successful at 5 years
1. HIV-positive patients receiving kidney transplants from HIV-positive donor patients experienced a 5-year cumulative survival of 74% and a 5-year cumulative graft survival of 84%.
2. After 5 years of follow-up, HIV-positive patients receiving kidney transplants from HIV-positive donors had viral load levels that remained undetectable.
Evidence Rating Level: 4 (Below Average)
Study Rundown: Kidney disease is a major problem affecting HIV-positive individuals, who now survive longer due to antiretroviral therapy (ART). Previous research has shown that outcomes of kidney transplantation are similar in HIV-negative and HIV-positive recipient when HIV-negative donor kidneys are transplanted. However, it is not known whether HIV-positive donor kidneys are a viable option for individuals requiring renal transplantation.
In this case series, 27 carefully selected HIV-positive patients received kidney transplants from HIV-positive donor patients. Pre-transplant, recipients received ART for at least 3 months, and had a CD4 T-cell count of 200 per cubic millimeter or higher and an undetectable plasma HIV RNA viral load. Patients with opportunistic infections were excluded. There was a cumulative patient survival of 84% at 1 year and 74% at 5 years; cumulative graft survival was 93% at 1 year and 84% at 5 years (if a patient died with a functioning graft, this was counted as if the graft had survived). HIV remained undetectable by standard testing in all recipients. Though not directly comparable given the study design, these results were similar to previous studies showing medium-term outcomes of HIV-negative kidneys transplanted into HIV-positive recipients.
This study proves the feasibility of using HIV-positive kidney donors for transplantation, an important finding for settings such as South Africa where the seroprevalence of HIV is high. However, the study did not compare outcomes from HIV positive and negative donors. Furthermore, the careful approach to designing the treatment protocol in order to optimize drug-drug interactions between the ART regimen and post-transplant immunosuppressive therapy would be hard to reproduce in a larger population or to implement at a system level.
Click to read the study, published today in NEJM
Click to read an accompanying editorial in NEJM
Relevant Reading: Outcomes of kidney transplantation in HIV-infected recipients
In-Depth [case series]: This prospective, nonrandomized case series involved 27 carefully selected HIV-positive patients in South Africa who received kidney transplants from HIV-positive donors. There were stringent selection criteria. Kidney recipients were HIV-positive and had been receiving ART for at least 3 months; had a CD4 T-cell count of 200 per cubic millimeter or higher and an undetectable plasma HIV RNA viral load. Patients with opportunistic infections were excluded, and those with a history of drug-sensitive tuberculosis were included only after completing at least 6 months of antibiotic treatment.
The cumulative patient survival was 84% (95% CI, 62 to 94) at 1 year and 74% (95% CI, 45 to 89) at 5 years; the rate of graft survival was 93% (95% CI, 74 to 98) at 1 year and decreased to 84% (95% CI, 55 to 95) at 5 years. The HIV viral load remained suppressed in all patients for the duration of follow-up. There were 8 cases of biopsy-confirmed acute rejection, with rejection rates of 8% at 1 year and 22% at 3 years. 6 of 8 episodes of acute rejection were successfully treated with immunosuppressive therapy.
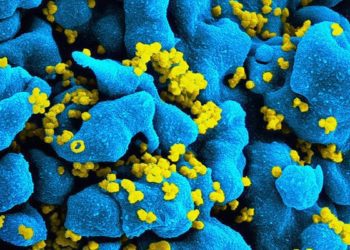
Image: PD/CDC
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.