Increased rates of unmet social needs observed shortly following a diagnosis of dementia
1. In this cohort study, dementia diagnosis was associated with increased levels of unmet social support needs, with notable differences based on race/ethnicity groups and sex.
Evidence Rating Level: 1 (Excellent)
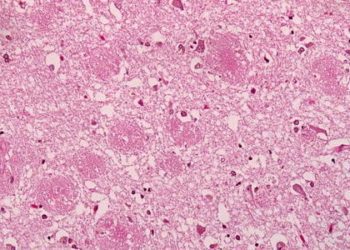
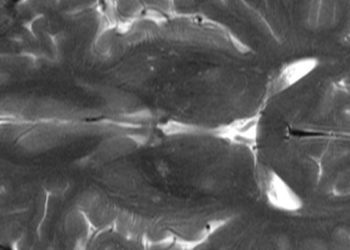
Dementia and cognitive impairment involve a decline in cognition and memory, gradually resulting in functional impairments including disorientation, communication difficulties, and impaired judgement. These impairments place a significant burden on the affected individuals, families, and the healthcare system. Past research has focused on care after hospital discharge, and there is limited quantitative evidence on support continuity following a dementia diagnosis, especially during transitions to community care. This study used data from the Health and Retirement Survey (HRS) with a matched ambidirectional cohort design to examine how unmet social support needs evolve before and after diagnosis. The exposure group consisted of individuals with a dementia diagnosis, while the control group consisted of individuals from the HRS with potential cognitive impairment but no confirmed dementia diagnosis. Unmet social support was characterized by the presence of physical disability in the absence of appropriate assistance. The total population included 1,261 individuals with a dementia diagnosis in the exposure group, and 12,604 individuals with possible cognitive impairment in the control group. Those in the exposure group experienced a significant increase in unmet support for instrumental activities of daily living (IADLs) (coefficient = 0.10, 95% CI [0.07, 0.13]), specifically for help with phone calls (coef = 0.74, 95% CI [0.16, 1.33]). When interpreting the results by race and ethnicity, there was a significant increase in unmet basic activities of daily living (BADLs) (coef = 0.74, 95% CI [0.03, 1.46]) specifically eating difficulties (coef = 1.58, 95% CI [0.17, 2.99]) in Hispanic individuals, and increase in unmet needs for toileting (coef = 1.52, 95% CI [0.57, 2.47]) and IADL support (coef = 0.09, 95% CI [0.00, 0.17]) in Black individuals. By sex, women had fewer unmet BADL (coef = -0.55, 95% CI [-1.03, -0.06]) needs but more unmet IADL support (coef = 0.08, 95% CI [0.04, 0.11]), while men had increased unmet needs for toileting (coef = 0.78, 95% CI [0.03, 1.53] and IADLs (coef = 0.14, 95% CI [0.10, 0.18]). Overall, these results indicate that a dementia diagnosis was associated with an increase in unmet social support, highlighting the need for more equitable care for people living with dementia to prevent the gaps from further increasing.
Image: PD
©2025 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.

![2 Minute Medicine: Pharma Roundup: Price Hikes, Breakthrough Approvals, Legal Showdowns, Biotech Expansion, and Europe’s Pricing Debate [May 12nd, 2025]](https://www.2minutemedicine.com/wp-content/uploads/2025/05/ChatGPT-Image-May-12-2025-at-10_22_23-AM-350x250.png)


![2MM: AI Roundup- AI Cancer Test, Smarter Hospitals, Faster Drug Discovery, and Mental Health Tech [May 2nd, 2025]](https://www.2minutemedicine.com/wp-content/uploads/2025/05/Untitled-design-75x75.png)

