Meta-analysis suggests endovascular therapy improves stroke outcomes
1. A meta-analysis of prospective randomized control trials of endovascular therapies for ischemic stroke demonstrated that endovascular therapies, when compared to standard medical management alone, improved patient outcomes at 90 days after intervention.
2. The demonstrated improvement of endovascular therapy over medical management was greatest among patients who had confirmed large vessel occlusion prior to treatment.
Evidence Rating Level: 2 (Good)
Study Rundown: To date, trials comparing endovascular therapy with medical management for acute ischemic stroke have failed to demonstrate superiority of either treatment. Many of these trials were criticized; however, for their use of older techniques and/or equipment, as well as for the subset of patients included in the treatment arms. In particular, stroke patients enrolled in prior multicenter trials often did not have large vessel occlusion (LVO) confirmed by imaging prior to intervention, and thus patient selection for endovascular therapy may have been suboptimal. More recent trials have begun to suggest improved outcomes using endovascular therapy, with the most recent being the Multicenter Randomized Clinical trial of Endovascular treatment for Acute Ischemic stroke in the Netherlands (MR CLEAN). In the present study, a meta-analysis was conducted using all prospective randomized controlled trials (RCTs) comparing endovascular therapy with medical management in the treatment of acute ischemic stroke. The study’s results suggested that patients who undergo endovascular therapy have better outcomes per the modified Rankin Scale (mRS)—a validated scale of post-stroke disability—than those who receive standard medical care. This finding was confirmed among patients both with and without confirmed LVO, though those with LVO confirmation had greater benefit. No difference in mortality was noted between the two treatment arms of the study, though there was a trend toward significance among those with LVO confirmation. These findings suggest a potential role for endovascular therapy in patients with acute ischemic stroke due to improved patient outcomes, something that was last advanced with the introduction of intravenous tissue plasminogen activator (tPA) use. This study was limited by the fact that the analyzed studies all involved different patient populations and utilized of inclusion criteria, creating a heterogeneous analysis group. In addition, the prospective cohorts being analyzed were generally small in size, with the largest being the most recent MR CLEAN cohort; this may have skewed results toward more recent findings. Future RCTs with a large patient population are warranted to validate these promising results.
Click to read the study in Journal of Neurointerventional Surgery
Relevant reading: Endovascular therapy after intravenous t-PA versus t-PA alone for stroke.
In-Depth [meta-analysis]: In this study, prospective RCTs of endovascular therapy for acute ischemic stroke were compared to standard medical management alone, which may have included peripheral intravenous tPA use. A total of 6 trials met full inclusion criteria. Following data aggregation, 2 separate data sets were compiled: one in which patients had confirmed LVO by imaging prior to intervention (n=1183), and a second including all patients regardless of LVO imaging confirmation (n=1903). The primary endpoint for both sets was an mRS of 0-2 at 90 days, scores indicating no disability or minor disability. Secondary outcomes included 90-day mRS of 0-1, 90-day mRS of 0-3, and overall mortality. Among those with LVO imaging confirmation, a significantly greater number of patients reached the primary endpoint following endovascular therapy when compared to patients assigned to medical management alone (OR 1.67, 95% CI 1.29-2.16, P=0.001). Similar results were obtained when patients without LVO confirmation were included in the analysis (OR 1.27, 95% CI 1.05 to 1.54, p=0.019). No difference in mortality was noted in either dataset; however, there was a trend toward significance among those with LVO confirmation when compared to those without.
More from this author: Magnetic resonance imaging may aid detection of pulmonary hypertension, Breast ultrasound may improve cancer detection in dense breasts, Optical molecular imaging improves lesion localization during liver procedures
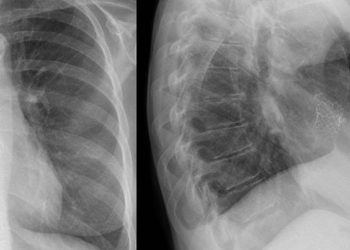
Image: PD
©2014 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. No article should be construed as medical advice and is not intended as such by the authors, editors, staff or by 2 Minute Medicine, Inc.