Neither haloperidol nor ziprasidone significantly shortens delirium in the ICU
1. Among critically ill patients with delirium in the intensive care unit (ICU), there was no significant difference in the duration of delirium between patients treated with haloperidol, ziprasidone, or placebo.
2. At the time of randomization, 89% of patients in the trial had hypoactive delirium versus only 11% that had hyperactive delirium.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Though primarily based on observational studies and expert recommendation, haloperidol and atypical antipsychotics are a standard therapy for delirium; however, the literature is conflicting about whether these medications are of benefit. The authors thus conducted this randomized trial to assess the efficacy of haloperidol and ziprasidone, a common atypical antipsychotic used to treat delirium, for the treatment of delirium during critical illness. The results showed no significant difference in the primary endpoint – days alive without delirium or coma – between the haloperidol, ziprasidone, or placebo groups. There was also no significant difference in the secondary endpoints, including days with delirium or coma and time to freedom from mechanical ventilation, ICU discharge, ICU readmission, and hospital discharge. Besides the higher incidence of prolongation of the corrected QT interval with ziprasidone, no significant differences in safety were reported between the three groups. While the results challenge the widespread use of antipsychotics to treat delirium in clinical practice, more data is needed to assess efficacy in hyperactive versus hypoactive delirium.
This was a randomized, double-blinded, placebo-controlled trial that assessed two of the most commonly used medications to treat delirium. Validated tools to assess delirium were used and high adherence to the trial protocol was reported. However, the high percentage of patients with hypoactive delirium limits the generalizability of the results, as the trial medications are more commonly used to treated hyperactive delirium. Additional limitations include that the trial was only powered to detect a 2-day difference between groups (thus any smaller difference is unknown) and the common co-administration of sedatives during the trial.
Click to read the study in NEJM
Relevant Reading: Effect of intravenous haloperidol on the duration of delirium and coma in critically ill patients (HOPE-ICU): a randomised, double-blind, placebo-controlled trial
In-Depth [randomized controlled trial]: Patients in the ICU on invasive mechanical ventilation, noninvasive positive pressure ventilation, vasopressor support, or intra-aortic balloon pump, who were determined to have delirium (n=566) were randomized to haloperidol (n=192), ziprasidone (n=190), or placebo (n=184). Delirium was detected using the Confusion Assessment Method for the ICU (CAM-ICU) validation tool and the Richmond Agitation-Sedation Scale (RASS) was used to determine hyperactive versus hypoactive delirium. Hyperactive delirium was detected in 11% of trial patients and 89% had hypoactive delirium. The primary endpoint was days alive without delirium or coma. Secondary efficacy endpoints included duration of delirium, time to freedom from mechanical ventilation, time to final successful ICU discharge, time to ICU readmission, and time to successful hospital discharge. Safety endpoints included the incidence of torsades de pointes and neuroleptic malignant syndrome.
The adjusted median number of days alive without delirium or coma was 8.5 in the placebo group (95% confidence interval [CI], 5.6 to 9.9), 7.9 in the haloperidol group (95% CI, 4.4 to 9.6), and 8.7 in the ziprasidone group (95% CI, 5.9 to 10.0) (P=0.26 across all groups). In the analyses of the trial-drug groups versus placebo, the 95% CI for the odds ratios included unity for days with delirium and coma during the 14-day intervention period, as well as time to freedom from mechanical ventilation, ICU discharge, ICU readmission, and hospital discharge in the 30-day and 90-day survival analysis. Prolongation of the corrected QT interval was more common in the ziprasidone group and torsades de pointes developed in two patients in the haloperidol group. No significant difference in the frequency of excessive sedation or other safety endpoint was noted.
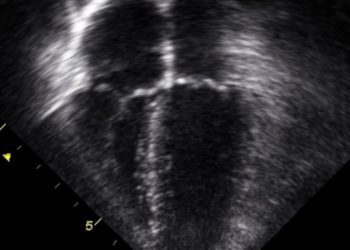
Image: PD
©2018 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.