Neoadjuvant pembrolizumab with chemoradiotherapy not supported for locally advanced rectal cancer after chemotherapy treatment
1. Although combining pembrolizumab to chemoradiotherapy as part of total neoadjuvant therapy after FOLFOX (5-fluorouracil, leucovorin, and oxaliplatin) treatment was safe overall, the difference in neoadjuvant rectal score does not support further study of this novel combination for the treatment of locally advanced rectal cancer.
2. These results and the high recurrence of metastatic disease among patients with locally advanced rectal cancer suggest that new agents and therapeutic combinations need to be explored.
Evidence Rating Level: 1 (Excellent)
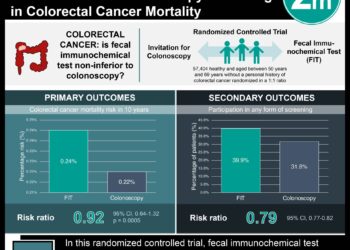
Study Rundown: Total neoadjuvant therapy (TNT) is an emerging option in cancer treatment that involves chemoradiation and chemotherapy prior to surgery to optimize the delivery of systemic therapy aimed at micrometastases. It is frequently used to downstage locally advanced rectal cancer (LARC) and decrease locoregional relapse. However, despite achieving low locoregional relapse rates in recent studies, 5-year overall survival (OS) remains poor, with more than one-third of patients developing recurrent metastatic disease. Therefore, novel agents and combinations with parallel, noncomparative experimental arms in LARC are needed. This randomized phase 2 clinical trial sought to evaluate whether the addition of pembrolizumab to neoadjuvant chemoradiotherapy improved efficacy compared to chemoradiotherapy alone for patients with LARC who have completed 4 months of neoadjuvant FOLFOX (5-fluorouracil, leucovorin, and oxaliplatin). The main outcome of this intent-to-treat analysis was the neoadjuvant rectal (NAR) score with a focus on end points recorded after definitive surgery including the NAR score, pathologic complete response (pCR) rate, sphincter-sparing surgery (SSS), clinical complete response rate, margin involvement, and safety. Secondary measures also included disease-free survival and OS. Among 185 patients with stage II/III LARC included in the study, the mean NAR score was 11.53 for the pembrolizumab cohort compared to 14.08 for the control. These results suggested that although pembrolizumab added to chemoradiotherapy as part of TNT was safe overall, the difference in NAR score does not support further study in combining neoadjuvant pembrolizumab with chemoradiotherapy after FOLFOX treatment of LARC. A limitation of this study was that although the original methods called for patients in both cohorts to receive similar exposures to chemoradiotherapy, 44 (54.3%) individuals did not receive all 6 doses of pembrolizumab and 23 (28.4%) patients received fewer than 5 doses, potentially reducing the consistency and generalizability of the study results.
Click to read the study in JAMA Oncology
In-Depth [randomized controlled trial]: This open-label, phase 2, randomized clinical trial enrolled a total of 185 patients from academic and private practice settings from August 2018 to May 2019 with analysis completed in August 2020 (126 [68.1%] male; mean [SD] age, 55.7 [11.1] years). Patients with stage II/III LARC with distal location (cT3-4 ≤5 cm from anal verge, any N), with bulky disease (any cT4 or tumor within 3mm of mesorectal fascia), at high risk for metastatic disease (cN2), and/or ineligible candidates for SSS were stratified based on clinical tumor and nodal stages. Patients were randomized (1:1) to the control arm (CA; n = 95) or the pembrolizumab arm (PA; n = 90) and received neoadjuvant FOLFOX for 4 months before undergoing chemoradiotherapy (capecitabine with 50.4 Gy) with or without intravenous pembrolizumab administered at a dosage of 200mg every 3 weeks for up to 6 doses before surgery. Among 137 patients evaluated for NAR score (68 CA and 69 PA patients), the mean (SD) NAR score was 11.53 (12.43) for the pembrolizumab cohort (95%CI, 8.54-14.51) vs 14.08 (13.82) for the control (95%CI, 10.74-17.43) (P = .26). The pCR rate was 31.9% and 29.4% for the PA and CA respectively (P = .75). The clinical complete response rate was 13.9% and 13.6% for PA and CA respectively (P = .95). The percentage of patients who underwent SSS was 59.4% and 71.0% for PA and CA respectively (P = .15). Lastly, grade 3 to 4 adverse events were slightly higher in PA (48.2%) compared to CA (37.3%) during chemoradiotherapy. Two deaths occurred during FOLFOX due to sepsis (CA) and pneumonia (PA). No differences in radiotherapy fractions, FOLFOX, or capecitabine doses were found.
Image: PD
©2021 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.