Patient Basics: Miscarriage
Originally published by Harvard Health.
What Is It?
- A miscarriage is a loss of a pregnancy. The term is generally used when the loss occurs before the fetus might be able to survive outside the womb, so before about 22 to 24 weeks of gestation. Other terms that are used for such losses include spontaneous abortion and early pregnancy failure.
- About 15% to 20% of known pregnancies end in a miscarriage. Most miscarriages happen before the pregnancy is 12 weeks along. In the first several weeks of a pregnancy, a miscarriage sometimes happens because a fertilized egg did not properly form a fetus. In many cases, the activity of the fetal heart stopped days or weeks before the symptoms of miscarriage began.
- A common sign of miscarriage is bleeding, although not all pregnancies with bleeding end in miscarriage.
- In the years before ultrasound, a miscarriage was diagnosed when a woman’s body had expelled all or some of the fetus, the placenta and the fluid surrounding the baby. Today, ultrasound may identify pregnancy loss before the body has begun the process of expulsion. Sometimes this finding is called a “miscarriage.”
- Miscarriages and possible miscarriages are categorized in several ways:
- Threatened miscarriage — A miscarriage is considered threatened or possible, when any bleeding from the uterus occurs before 20 weeks but the cervix is closed and there is evidence of continued fetal heart activity.
- Inevitable abortion or miscarriage — A miscarriage is called inevitable, meaning it cannot be stopped, if there is bleeding from the uterus and the cervix is opening prior to 20 weeks, but neither the fetus nor placenta has passed out of the woman’s body yet. The membranes around the fetus may or may not have ruptured (broken).
- Incomplete abortion or miscarriage — A miscarriage is incomplete when a portion of the fetus or placenta has passed out of the uterus prior to 20 weeks gestation, but some of the placental or fetus remains in the uterus.
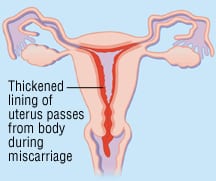
- Complete miscarriage — A miscarriage is complete if the fetus, all the membranes around the fetus and the placenta are expelled completely and the cervix closes prior to 20 weeks.
- Missed abortion or miscarriage — A missed abortion refers to a miscarriage in which the fetus has died prior to 20 weeks gestation, but neither the fetus nor the placenta has been expelled from the uterus.
- Recurrent miscarriage — A woman is said to have recurrent miscarriage after three or more miscarriages in a row. Approximately 1% of women experience recurrent miscarriages.
- Blighted ovum or anembryonic gestation — This occurs when a gestational sac forms inside the uterus, but no fetus is present after seven weeks.
If a pregnancy ends after 20 weeks, it is not considered a miscarriage. The fetus gets delivered, and if the fetus is not living, the event is called a stillbirth.
Problems with fetal chromosomes account for approximately 50% of all miscarriages. Chromosomes are long strings of DNA, each containing thousands of genes. Genes, in turn provide the instructions for the proteins and other molecules that create, shape and govern our bodies and health.
In most cases, the abnormalities of chromosomes that caused a miscarriage do not reflect any abnormality in either parent. Instead they reflect problems that developed at the time the egg or sperm developed, or at the time when fertilization and early division of the fertilized egg took place. In these case, where the miscarriage is related to chromosomal abnormalities, many think of it as the body’s way of ending a pregnancy that is not developing normally.
In some unusual circumstances, miscarriages can happen if there are problems with the internal structure of a woman’s uterus or the function of her cervix.
Infections such as rubella (German measles) have been associated with miscarriage. This has led some to wonder if there are other infections that cause early pregnancy loss, but few links have been confirmed. Some experts have also suggested that hormonal imbalances can result in miscarriage, but identifying specific abnormalities has proven difficult.
In rare cases, a woman’s immune system appears to react with the pregnancy tissue, resulting in miscarriage. Overall, immune system disorders seem to be responsible for very few miscarriages, but among women who have had three or more miscarriages in a row (recurrent miscarriage), immune-system disorders are responsible for 5% to 10% of these losses. One fairly common antibody problem that can lead to recurrent miscarriage is called “antiphospholipid antibody syndrome.” Another example of an immune related issue associated with miscarriage is the production of antibodies that react to the thyroid gland (thyroperoxidase antibodies).
Having either type of antibody is unusual. But it may be more common when there have been several miscarriages (recurrent miscarriage). Testing for such antibodies after several miscarriages is often suggested. Treatment for the antibody disorders may decrease the risk of future miscarriage.
In many cases, no cause for a miscarriage is identified.
Symptoms
Symptoms of miscarriage include:
- Vaginal bleeding that may start as a brownish discharge. When bleeding is heavy there may be blood clots or other tissue passing from the vagina. However, not all bleeding during a pregnancy means that a miscarriage is happening
- Cramps or other pain in the pelvic area, lower back or abdomen
- A decrease in the usual signs of early pregnancy, such as nausea and breast tenderness. However, such symptoms normally disappear in healthy pregnancies. So, their disappearance only rarely signifies miscarriage.
In addition to the possibility of miscarriage, pain or vaginal bleeding during pregnancy can be caused by other problems, such as a tubal (ectopic) pregnancy. These symptoms should always prompt an immediate call to your doctor, midwife or nurse practitioner.
Diagnosis
If miscarriage is suspected or has occurred, an ultrasound and pelvic exam are usually performed. Your doctor, midwife or nurse will do a pelvic examination to check the size of your uterus and determine whether your cervix is open or closed. If a miscarriage is in progress, the cervix is usually open and the pregnancy will not survive. If a miscarriage has already happened, the cervix can be either open or closed, depending on whether all the pregnancy tissue has passed out of the womb.
Blood tests are usually done to verify your blood type and check the level of human chorionic gonadotropin (beta-hCG), a hormone released by the placenta into your body when you are pregnant. If the amount of the pregnancy hormone in your system is low or if repeated tests show the level has decreased over time, this is a sign you may have had a miscarriage.
In many cases when symptoms indicate a miscarriage, the evaluation will include or even start with an ultrasound. An ultrasound is used to identify if a fetus is present or if the fetal heart is beating. Together with the results of blood tests, ultrasound results can help your doctor evaluate the health of a pregnancy and consider other diagnoses such as tubal pregnancy.
If pregnancy tissue has passed out of your vagina, you can bring it to your doctor in a glass jar or plastic container with a tightly sealed lid. It may be helpful for your doctor to inspect this tissue, although this is not a necessary step for diagnosing a miscarriage. In some cases, this tissue can be sent to a laboratory to be examined under a microscope.
Expected Duration
Once bleeding has started and a miscarriage has begun or a loss been diagnosed (for example, an incomplete or missed miscarriage, it is difficult to predict how long bleeding will continue and how long it will take for all the tissue to pass, or even if it will all pass without assistance. In many cases, all the pregnancy tissue will pass without intervention. In these cases, bleeding and cramps will gradually decrease over one to two weeks. Miscarriages that occur in the second trimester may be followed by a longer time of bleeding. When medications or procedures are used to remove the tissue, the specific treatments used and their timing will determine the duration of symptoms.
Prevention
If a miscarriage is about to occur, you usually can’t prevent it. In the past, if there were bleeding early in a pregnancy and the diagnosis of a threatened miscarriage were made, reduced activity or even bed rest would be recommended. Now, most doctors recognize that there is little evidence that such measures, or indeed any intervention, reduce the risk of miscarriage.
However, you may be able to decrease your chances of having a miscarriage in a future pregnancy by taking good care of yourself, eating a healthy diet, taking folic acid supplements, exercising regularly and not smoking. If you have any diseases going into your pregnancy, it’s best to work with your doctor to create a treatment plan that keeps you and the fetus as safe and healthy as possible. Note that miscarriage is not caused by regular physical activities, minor accidents, exercise, sexual intercourse, or minor stumbles or falls.
If you have had several miscarriages in a row, your doctor may recommend that you and your partner undergo a detailed evaluation to help identify, if possible, reasons for recurrent miscarriage.
Treatment
If you have a missed or incomplete miscarriage early in pregnancy, there are three options for management. The first option involves what is often termed “expectant management”: watching carefully for problems but letting tissues pass on their own. If bleeding is heavy, pain severe, or expectant management is unappealing, you and your obstetrician/gynecologist (OB/GYN) may choose to precede with a surgery called a dilation and curettage (D & C) to gently stretch open your cervix and remove any remaining fetal tissue from your uterus. A third option for managing first trimester losses involves using medicines placed in the vagina (most often by you at home) to promote the passage of tissue. This last option means less time spent waiting than with expectant management, and in most cases avoids procedures such as D&C. You and your providers can discuss which option is best for you.
For losses after the first trimester (first 12 weeks) D&C is often recommended. Rarely, induction of labor may be recommended. This is more likely if the cervix is already widely opened or if loss occurs closer to 20 weeks, Such second trimester procedures (particularly induction of labor) may require a longer stay in the hospital than that needed to manage a first trimester loss.
When To Call A Professional
Call the health care professional who is monitoring your pregnancy immediately if you have symptoms of a miscarriage, such as vaginal bleeding or persistent pain in your pelvis, abdomen or back.
Prognosis
Your chances of having another miscarriage depend on the cause of your first miscarriage. Because, as noted above, miscarriages occur in 15% to 20% of pregnancies, even a healthy couple has a 15% to 20% chance of a miscarriage in any pregnancy.
The general recommendation for attempting pregnancy after a miscarriage is to wait about two to three months before trying to conceive again, but if conception occurs sooner, there is not any marked increase in risk. For many, the answer to the question “when to try again” is related not to one’s body, but to the emotional recovery after enduring the loss of miscarriage.
It’s normal and common to feel sad, grief-stricken, and depressed after a miscarriage. Your doctor can suggest resources for support during this difficult time.
Additional Info
American College of Obstetricians and Gynecologists
409 12th St., SW
P.O. Box 96920
Washington, DC 20090-6920
Phone: (202) 863-2518
http://www.acog.org/
American College of Nurse Midwives
818 Connecticut Ave., NW
Suite 900
Washington, DC 20006
Phone: (202) 728-9860
Fax: (202) 728-9897
http://www.midwife.org/
National Institute of Child Health and Human Development
Building 31
Room 2A32
MSC 2425
31 Center Drive
Bethesda, MD 20892-2425
Phone: (301) 496-5133
Toll-Free: (800) 370-2943
http://www.nichd.nih.gov/
National Institute of Diabetes and Digestive and Kidney Disorders
Office of Communications and Public Liaison
Building 31, Room 9A04
Center Drive, MSC 2560
Bethesda, MD 20892-2560
Phone: (301) 496-3583
Fax: (301) 496-7422
http://www.niddk.nih.gov/