Patient-reported outcomes differ significantly based on treatment in prostate cancer: The ProtecT trial
1. Patients undergoing prostatectomy for prostate cancer had significantly worse self-reported urinary and sexual function compared to radiotherapy and active monitoring, whereas those undergoing radiation therapy had significantly worse bowel function.
2. No significant differences were found between measures of general health between the three treatment options.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Management of prostate cancer based on prostate-specific antigen (PSA) levels is a controversial issue in men’s health. Early detection and treatment may provide individual and population health benefits, but current treatment options have a significant negative impact on a patient’s quality of life.
The ProtecT trial compared the effectiveness and health outcomes between the three most common current treatments – prostatectomy, radiotherapy, and active monitoring. The primary outcome was mortality which was reported elsewhere. This study reports the secondary outcome of interest – patient-reported outcomes – including measures of urinary, sexual, and bowel function, as well as measures of general health. Prostatectomy was found to have the greatest negative effect on urinary and sexual function, while radiotherapy had the greatest negative effect on bowel function. No significant differences between treatments were found in measures of general health. In conjunction with mortality data provided in the companion study, this provides an appreciation of the risk-benefit tradeoff in managing patients with prostate cancer.
This was a large, randomized trial that used validated patient-reported outcomes and had high response rates. This trial was also used in a larger trial evaluating the effectiveness of PSA for prostate cancer screening, increasing its generalizability. Significant limitations include poor representation of nonwhite males and the introduction of new diagnostic and therapeutic techniques since the trial’s inception.
Click to read the study, published today in NEJM
Relevant Reading: 10-year outcomes after monitoring, surgery, or radiotherapy for localized prostate cancer
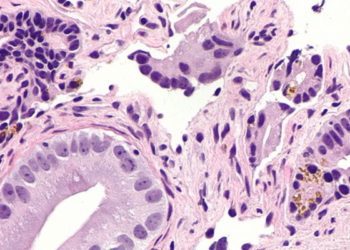
In-Depth [randomized controlled trial]: In this randomized trial, population-based PSA screening identified 1643 men with localized prostate cancer that were randomized to active-monitoring (n = 545), radical prostatectomy (n = 553), or radiotherapy (n = 545). The primary outcome (mortality due to prostate cancer or treatment at 10 years), evaluated in a separate analysis, found low levels of death due to prostate cancer (1%) irrespective of treatment, but reported a significantly lower rate of disease progression in the prostatectomy and radiotherapy groups compared to active monitoring (p < 0.001).
The secondary outcome of interest (patient-reported outcomes) described in this study used validated questionnaires based on four domains – urinary function, sexual function, bowel function, and health-related quality of life. Questionnaires were completed at baseline, 6 months and 12 months, and then annually for the 6 years of follow-up. At all time points, prostatectomy had a greatest negative effect on urinary continence (p < 0.001) and erectile function (p < 0.001). In the prostatectomy, radiotherapy, and active monitoring groups, respectively, the rate of absorbent pad use was 17%, 4%, and 8% at 6 months. Sexual function (based on erection firmness and sexual function scores) was reduced from 67% at baseline to 12%, 22%, and 52%, respectively. Bowel function (based on loose and bloody stool reports) was significantly reduced in the radiotherapy group compared to the other treatments (p < 0.001). No significant differences in health-related quality of life measures were found at any time point.
Image: CC/Wiki
©2016 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc

![2 Minute Medicine: Pharma Roundup: Price Hikes, Breakthrough Approvals, Legal Showdowns, Biotech Expansion, and Europe’s Pricing Debate [May 12nd, 2025]](https://www.2minutemedicine.com/wp-content/uploads/2025/05/ChatGPT-Image-May-12-2025-at-10_22_23-AM-350x250.png)