Self-perceived stress associated with increased risk of cryptogenic ischemic stroke
1. Self-reported stress levels are significantly associated with cryptogenic ischemic stroke in women and young adults (18-39 years old), representing an actionable, modifiable stroke risk factor
Evidence Rating Level: 2 (Good)
Study Rundown: Despite the evidence showing traditional vascular risk factors are associated with early-onset ischemic stroke, a significant proportion of young people experience cryptogenic strokes. This case-control study aimed to characterize the role of psychosocial stress as a possible modifiable risk factor. In post-stroke patients aged 18-49, self-perceived stress was assessed using the Perceived Stress Scale (PSS). The study found higher self-perceived stress was strongly associated with ICS. This association was more pronounced in women who showed significant association after controlling for vascular risk factors. Statistical significance was not reached in male participants. Similarly, there was a significant association between stress and CIS in younger patients (18-39 years old) but not older patients (40-49 years old). Overall, study findings underscore the significant association between self-perceived stress and early-onset CIS, particularly in young women. These findings highlight the importance of integrating stress assessment and management into stroke prevention strategies for young adults. Further research is needed to unravel the biological pathways linking stress to stroke and to develop targeted interventions aimed at reducing stress-related vascular risk.
Click to read the study in Neurology
Relevant Reading: Modern approaches to conceptualizing and measuring human life stress
In-Depth [case-control study]: The traditional vascular risk factors associated with strokes such as hypertension, smoking, and obesity are well-documented contributors to early-onset ischemic stroke (IS). However, a significant proportion of younger patients experience strokes with undetermined causes—termed cryptogenic ischemic strokes (CIS). Increasing evidence points to psychosocial stress as a potentially modifiable risk factor, prompting further investigation into its role in CIS.
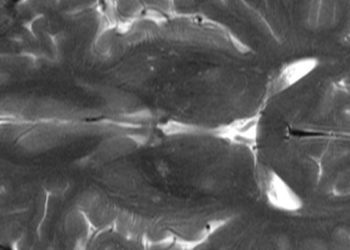
This multicenter case-control study drew participants from 19 European centers as part of the SECRETO study. It included 426 young patients (18-49 years old) with first-ever CIS and 426 age- and sex-matched stroke-free controls. CIS was confirmed through MRI or CT angiography after ruling out known causes of stroke. Self-perceived stress was assessed using a modified version of the Perceived Stress Scale (PSS), categorizing stress levels as low (0–13), moderate (14–26), and high (27–40). Researchers conducted conditional logistic regression analyses, adjusting for age, education level, and traditional vascular risk factors (including hypertension, diabetes, smoking, obesity, diet, physical inactivity, depression, and migraine with aura). The study found a strong independent association between higher self-perceived stress and early-onset CIS. Patients with CIS were more likely to report at least moderate stress compared to controls (46.2% vs. 33.3%, p < 0.001). Each 1-point increase in the PSS score was linked to a 4% increase in the odds of CIS (OR 1.04; 95% CI 1.01–1.07). When analyzing stress categories, moderate stress was significantly associated with CIS (OR 1.47; 95% CI 1.00–2.14), but high stress, though suggestive of a stronger effect (OR 2.62; 95% CI 0.81–8.45), did not reach statistical significance, likely due to fewer participants reporting extreme stress levels. Notably, the association was more pronounced in women. Among female participants, moderate stress remained a significant predictor of CIS even after adjusting for vascular risk factors and migraine with aura (OR 1.78; 95% CI 1.07–2.96). A 1-point increase in PSS was also linked to CIS in women (OR 1.06; 95% CI 1.02–1.11). In contrast, no significant relationship was found between stress and CIS in men after full adjustment for confounding factors. Age-stratified analysis revealed that higher perceived stress was significantly associated with CIS in younger participants aged 18–39 years (OR 1.06 per 1-point increase; 95% CI 1.00–1.11), but not in those aged 40–49 years after adjusting for vascular risks. This suggests that stress may exert a stronger influence on stroke risk in younger adults, potentially due to fewer competing risk factors. The authors highlight several potential mechanisms by which stress may contribute to stroke risk, including chronic inflammation, endothelial dysfunction, platelet activation, and autonomic dysregulation. Psychological stress can also induce a hypercoagulable state through increased levels of fibrinogen, von Willebrand factor, and other procoagulants. While this study has key strengths such as its large, multicenter design, comprehensive diagnostic workup for CIS, and use of validated stress measures, there is the risk of recall since stress was assessed post-stroke.
Image: PD
©2025 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.



![2 Minute Medicine: Pharma Roundup: Price Hikes, Breakthrough Approvals, Legal Showdowns, Biotech Expansion, and Europe’s Pricing Debate [May 12nd, 2025]](https://www.2minutemedicine.com/wp-content/uploads/2025/05/ChatGPT-Image-May-12-2025-at-10_22_23-AM-75x75.png)


