2 Minute Medicine Rewind February 27, 2017
Assessing the Risks Associated with MRI in Patients with a Pacemaker or Defibrillator
Patients with implanted cardiovascular electronic devices, such as pacemakers or defibrillators (ICD), often face safety concerns when requiring MRI images, often excluding these patients from MRI studies. This prospective cohort study, MagSafe Registry, identified 1500 patients with “non-MRI-conditional” devices, 1000 with pacemakers and 500 with ICDs, who had an indication for a non-thoracic MRI with field strength of 1.5T and determined the risks associated with it. Primary outcomes included death, generator or lead failure, induced arrhythmia, loss of capture, or electrical reset during the scanning. 75% of MRI scans were of brain or spine imaging. No deaths, lead failures requiring immediate replacement, ventricular arrhythmias, or loss of capture occurred during any of the 1500 MRI examinations. There were 6 observed atrial arrhythmias, 5 in pacemaker group (0.5%, 95% CI: 0.2 to 1.2%) and 1 in the ICD group (0.2%, 95% CI: 0.04 to1.1%). In 6 pacemakers (0.6% 95% CI: 0.1 to 1.3%), there was a partial electrical reset in patients that had the device planted 5.7 to 9.7 years before the MRI, while no full resets occurred. A small percentage of showed changes in pacing threshold, lead impedance, R-wave and P-wave amplitude reductions, and battery voltage. Limitations of this study include the variability of manufacturers of leads and generators. Nonetheless, this study reveals that patients with adequately screened and reprogrammed devices showed no adverse effects after 1.5T MRI.
Association of Testosterone Levels with Anemia in Older Men
Anemia is present is approximately 10% of older adults, and prior studies have shown that low testosterone levels were significantly related to unexplained anemia in men. In this double-blinded placebo-controlled study, 783 men aged 65 or older, with at least two serum testosterone measurements less than 275 ng/dL and hemoglobin levels between 10.0 – 12.5 g/dL, were enrolled in the Anemia Trial and given either placebo or testosterone gel titrated to normal range for young, normal men. In patients with unexplained anemia, testosterone treatment was significantly related to improved hemoglobin of at least 1.0 g/dL (AOR: 31.5; 95% CI: 3.7 to 277.8, p = 0.002) compared to placebo, as well as in patients with anemia of known cause (AOR: 8.2; 95% CI: 2.1 to 31.9; p = 0.003) and non-anemic men (OR: 20.7; 95% CI: 12.9 to 33.3; p < 0.001). A majority of men at 12 months were also no longer anemic (anemia of unknown cause 58.3%, anemia of known cause 60%). This increase of 1.0 g/dL of hemoglobin was also associated with an improvement in 6-minute walk distance by 8.3m (p < 0.001) and improved perceived health status. In the non-anemic group, 6 patients (1.7%) developed erythrocytosis. Limitations include a small sample size for each anemia group, and does not account for men under 65 with unexplained anemia. Ultimately, the use of testosterone may help improve anemia, but must be evaluated with overall health benefits.
Bleeding during high-risk cardiac surgeries, with some 15% to 20% of patients consuming 80% of blood products used in cardiac surgery, is frequently treated with coagulation factor replacement. With major blood loss, red blood cells and colloid fluids are often given, leading to an early plasma fibrinogen deficiency which may lead to further postoperative blood loss. In this randomized clinical trial, 120 adults who were undergoing elective high-risk cardiac surgery, including coronary artery bypass graft (CABG), valve repair or replacement, replacement of multiple valves, aortic root reconstruction, or reconstruction of ascending aorta or aortic arch, were randomized to receive either placebo or fibrinogen during surgery to study the outcome of intraoperative blood loss, along with postoperative blood loss. 72% of patients underwent CABG with combined valve replacement/repair, and had similar preoperative plasma fibrinogen levels (intervention group 2.9 g/L vs. placebo group 2.8 g/L). There was no significant difference in blood loss from time of fibrinogen infusion to chest closure in intervention group (median, 50 mL; IQR: 29-100 mL) and the control group (median, 70 mL; IQR: 33-145 mL; p = 0.19); after controlling for age, sex, EuroSCORE, lowest core temperature, and cardiopulmonary bypass time no significant difference was observed (p = 0.09). Fewer patients in the fibrinogen group were given blood products, although the study was not adequately powered to draw significant conclusions. Adverse events were more prevalent in the fibrinogen group vs. placebo including death (2 vs. 0 patients), strokes or transient ischemic attacks (4 vs. 2), and myocardial infarctions (3 vs. 1). Further regression analysis of cumulative blood loss in first 24 hours after surgery showed a reduction in blood loss in fibrinogen group of 570 mL (IQR, 390-730 mL) compared with placebo of 690 mL (IQR, 400-1090 mL; p = 0.047). This single center study may not be generalizable. Overall, the use of fibrinogen in high-risk cardiac surgery resulted in no significant difference in blood loss compared to placebo.
Bariatric Surgery versus Intensive Medical Therapy for Diabetes — 5-Year Outcomes
Bariatric surgery has shown promise in treatment of type 2 diabetes patients with mild to moderate obesity, in comparison to intensive medical therapy. The STAMPEDE trial completes the 5-year follow-up in confirming superiority of bariatric surgery in achieving glucose control and sustained weight loss. In this randomized, controlled, non-blinded single-center trial of 134 patients with HbA1C level greater than 7.0% and a body-mass index (BMI) of 27 to 43, participants were randomized to either intensive medical therapy alone, intensive medical therapy plus gastric bypass or sleeve gastrectomy, and stratified by baseline use of insulin. Primary outcome was HbA1C level of 6.0% or less with or without the use of diabetes medications. In the 5-year follow up, patients achieving the primary outcome were greater with gastric-bypass (29% vs. 5%; p = 0.01) and sleeve gastrectomy (23% vs. 5%; p = 0.03) compared to medical therapy alone. A duration of diabetes less than 8 years (p = 0.007) and random assignment to gastric bypass alone (p = 0.03) were significant predictors of achieving HbA1C less than 6.0%. Weight loss reduction was greater in gastric bypass than sleeve gastrectomy (p = 0.01), nonetheless, reductions in body weight, BMI, waist-to-hip ratio, and waist circumference were greater in surgical therapy than medical therapy (p <0.05 for all comparisons). Additional secondary outcomes revealed a significant reduction of triglycerides, increase of high-density lipoprotein, and improvement of pain and quality of life surveys (p < 0.05 for all comparisons) with surgical therapy. No significant differences were noted with low-density lipoprotein, blood pressure, renal, or ophthalmologic outcomes. Bariatric surgery plus intensive medical therapy showed more effective than medical therapy alone among type 2 diabetes patients with BMI between 27 and 43.
Peritoneal Dialysis vs Furosemide for Prevention of Fluid Overload in Infants After Cardiac Surgery
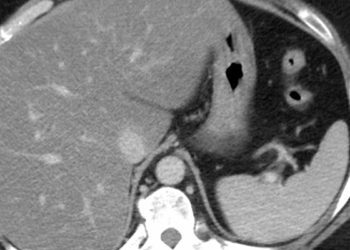
After congenital heart surgery in infants, fluid overload is a notable cause of morbidity and mortality, caused by impaired hemodynamics, acute kidney injury, and capillary leak. Peritoneal dialysis (PD) has been used safely, but has not previously been compared to standard diuretic treatment. In this randomized clinical trial, 73 infants under 6 months undergoing cardiac surgery with cardiopulmonary bypass were given either PD or furosemide administration to study primary outcomes of the percentage of patients with a negative fluid balance on post-operative day (POD) 1, calculated as the net difference between all inputs and outputs. Median age of patients was 8 days (IQR 6 – 14 days). Patients on PD had no significant different in the proportion achieving a negative fluid balance on POD 1 compared to patients on furosemide (29 of 41 [71%] vs 21 of 32 [66%]; p = 0.80). Patients on furosemide were 3 times more likely to develop 10% fluid overload (OR, 3.0; 95% CI: 1.3 – 6.9). Also, patients in PD group reached the net negative fluid balance 1 shift sooner and had better median fluid balances on POD 1 (55 mL [IQR, −25 to 194] vs 118 [IQR, 51 to 197] mL). Patients on furosemide were also more likely to received prolonged mechanical ventilation (OR, 3.1; 95% CI: 1.2 – 8.2). PD patients had 1.5 days shorter of inotropic agent infusions, and fewer electrolyte repletion doses. Patients did not significantly differ in duration of cardiac ICU care, or in-hospital mortality. Two PD – related adverse outcomes occurred, but not peritonitis or bowel injury. Limitations include small study size and single study site limiting its generalizability. Nonetheless, the study reveals that PD in infants is a safe and superior method for prevention of fluid overload, especially infants at high risk for AKI and subsequent fluid overload, following cardiac surgery.
Image: PD
©2017 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.