2 Minute Medicine Rewind January 10, 2022
Atorvastatin versus placebo in patients with covid-19 in intensive care: randomized controlled trial
1. There was no difference in thrombotic events or 30-day all-cause mortality for COVID-19 ICU patients treated with 20 mg atorvastatin daily compared to placebo.
Evidence Rating Level: 1 (Excellent)
COVID-19 patients, particularly those in the intensive care unit (ICU), are at risk for thrombosis-related mortality, due to endothelial dysfunction and immobility. Statins have anti-inflammatory, anti-oxidant, and anti-thrombotic effects, and have shown to reduce vascular events such as venous thromboembolism. Therefore, the goal of this randomized controlled trial was to determine if 20 mg atorvastatin daily, compared to placebo, would be safe and effective at reducing thrombotic events and mortality in COVID-19 ICU patients. The study population consisted of COVID-19 positive ICU patients who had no clear indication for anticoagulants or statins. These patients were recruited from 11 hospitals in Iran: 219 were randomized to placebo, and 215 randomized to atorvastatin. The primary outcome encompassed presence of venous or arterial thrombosis, treatment with extracorporeal oxygen, and all-cause mortality with a 30-day follow-up after randomization. The results found that the primary outcome was not different in the two groups, occurring in 36% of the placebo group and 33% of the atorvastatin group (odds ratio 0.84, 95% CI 0.58-1.21, p = 0.35). The primary outcome was mostly due to 30-day all-cause mortality, with 35% in the placebo and 31% in the atorvastatin group (OR 0.84, 95% CI 0.58-1.22), since no patient was treated with extracorporeal oxygen. With regards to safety, liver enzymes increased to 3 times the upper limit of normal in 2% of placebo and atorvastatin patients respectively (OR 0.85, 95% CI 0.25-2.81, p = 0.79), and major bleeding also did not differ, occurring in 2% of placebo and 4% of atorvastatin patients (OR 2.30, 95% CI 0.78-6.73, p = 0.12). Overall, this study found no difference in thrombotic events and all-cause mortality for COVID-19 ICU patients treated with atorvastatin versus placebo.
1. Drug-eluting stents (DESs) had a lower risk of in-stent restenosis (ISR) and ischemic stroke recurrence compared to bare-metal stents (BMSs) for patients with high-grade symptomatic intracranial atherosclerotic stenosis (ICAS).
Evidence Rating Level: 1 (Excellent)
Intracranial atherosclerotic stenosis (ICAS) causes 8-10% of strokes in North America and 30-50% of strokes in Asia. Medical therapy is the standard treatment for ICAS, while intracranial stenting is considered an inferior option due to complications. For example, in-stent restenosis (ISR) occurs in 15-33% of patients within a year of receiving a bare-metal stent (BMS). Drug-eluting stents (DESs) are recommended over BMSs, as they inhibit endothelial cell migration and have reduced ischemic events for coronary artery disease. However, only retrospective case studies have compared the two stent types. Therefore, this randomized controlled trial aimed to compare the risk of ISR in DESs and BMSs, for patients with high-grade symptomatic ICAS. The study population consisted of 263 patients recruited from 16 medical centres in China. These patients all had a transient ischemic attack or nondisabling ischemic stroke, with 70-99% stenosis on angiography. 132 were randomized to the DES group, and 131 were randomized to BMS. All patients received dual antiplatelet therapy (aspirin and clopidogrel) 5 days prior to and 90 days after the procedure, before switching to one medication only. The results found no difference in stroke or mortality after 30-day follow-up, with 7.6% in the DES group and 5.3% in the BMS group (odds ratio 1.45, 95% CI 0.54-3.94, p = 0.46). The rates for intracranial hemorrhage were around 0.5 times higher in the DES group (4.5% versus 3.1%) and around twice higher for disabling or fatal stroke in the DES group (4.6% versus 2.3%), but was not significantly different for either outcome. However, ISR was significantly lower in the DES group, occurring in 9.5% of DES patients and 30.2% of BMS patients (OR 0.24, 95% CI 0.11-0.52, p < 0.001). The rate of ISR was also lower at 1-year follow-up in the DES group, with 9.9% of DES patients compared to 26.7% of BMS patients (OR 0.22, 95% CI 0.09-0.52, p < 0.001). The DES group also had a reduced risk of ischemic stroke from Day 31 to 1 year of follow-up, with 0.85% of patients compared to 6.9% in the BMS group (hazards ratio 0.10, 95% CI 0.01-0.80, p = 0.03). Overall, this study demonstrated that DESs had a lower risk of ISR and ischemic stroke recurrence compared to BMSs, for patients who had a high-grade ICAS.
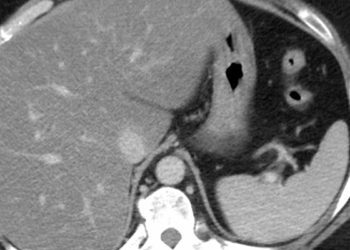
1. Patients receiving non-living donor livers preserved with normothermic perfusion had lower rates of early allograft dysfunction (EAD) and ischemic biliary complications (IBCs), compared to donor livers preserved with ischemic cold storage (ICS).
Evidence Rating Level: 1 (Excellent)
The current method for donor liver preservation is ischemic cold storage (ICS). However, ICS is associated with ischemic injury and deterioration of the donor organ, and also does not allow the quality of the organ to be assessed prior to implanting. These factors lead to an underusage of liver allografts: Donated organs from patients with advanced age or comorbidities are often declined due to a concern for early allograft dysfunction (EAD) and ischemic biliary complications (IBCs). A proposed alternative to ICS is normothermic blood-based liver perfusion, which perfuses the organ with warm, oxygenated, blood. This alternative minimizes the duration of ischemia and allows for an assessment of the donor organ function. The current study is the first muluti-centre randomized controlled trial in the United States comparing the effectiveness of ICS versus liver perfusion, which was referred to as the Portable Organ Care System (OCS). The study used non-living donor livers that were considered more vulnerable, including livers from patients 40 years or older, that had an expected ischemic time of 6 or more hours, that were from patients 55 years and younger donated after brainstem death (DBD), or were macrosteatotic. There were 293 organ recipients, with 142 randomized to the ICS group and 151 to the OCS group. The primary outcome was the incidence of EAD in the first 7 post-operative days. The results showed that donor livers in the OCS group were perfused for a mean (SD) time of 276.6 (117.4) minutes, and reduced the mean (SD) cold ischemia time to 175.4 (43.5) minutes compared to 338.8 (91.5) minutes for ICS. Furthermore, the OCS group had a significantly lower incidence of EAD (18%) in the per-protocol analysis, compared to 31% in the ICS group (p = 0.01). Biopsies following reperfusion were done, and there was significantly fewer livers with lobular inflammation (a marker of ischemia-reperfusion damage) in the OCS group (6% versus 13%, p = 0.004). As well, OCS livers were associated with significantly fewer IBCs at 6 months (1.3% versus 8.5%, p = 0.02) and at 12 months (2.6% versus 9.9%, p = 0.02). In conclusion, patients receiving donor livers preserved with normothermic perfusion had less dysfunction and fewer complications, compared to donor livers preserved with ischemic cold storage.
1. There was no association between a healthy or unhealthy plant-based diet and cardiovascular disease (CVD) or all-cause mortality, over 15-year follow-up for an African American cohort.
Evidence Rating Level: 2 (Good)
Plant-based diets have been associated with a lower risk of heart disease through observational studies, but findings have been mixed when it comes to prospective studies. One reason may be that the overall healthiness of a plant-based diet is variable, so studies have stratified plant-based diets into healthy or unhealthy. A limitation of plant-based diet research is that the African American population is understudied. Therefore, this prospective study used the Jackson Heart Study cohort, one of the largest African American study cohorts in the USA, to evaluate the association between cardiovascular disease (CVD) and 3 categories of plant-based diets: Healthy, unhealthy, and overall plant-based diets. The study population consisted of 3,635 African Americans in Jackson, Mississippi, from 21-95 years of age, who had no history of CVD or stroke at baseline. The participants’ diet was assessed through a Food Frequency Questionnaire, and plant-based diet indices (PDIs) were established, including an overall PDI, a healthy PDI (hPDI), and an unhealthy PDI (uPDI). Healthy plant groups included whole grains, fruits, and veggies, whereas unhealthy groups included potatoes, fruit juices, sugary drinks, and sweets. The results showed that over a median 15-year follow-up, the incidence of CVD and all-cause mortality did not differ based on PDI score, for any of the 3 indices. For instance, the hazard ratios for incidence of CVD for the highest, compared to lowest, tertiles of overall PDI, hPDI, and uPDI were 1.06 (95% CI 0.78-1.42, p-trend = 0.72), 1.07 (95% CI 0.80-1.42, p-trend = 0.67), and 0.95 (95% CI 0.71-1.28, p-trend = 0.76) respectively. For all-cause mortality, the HRs were 0.96 (95% CI 0.78-1.18, p-trend = 0.67), 0.94 (95% CI 0.76-1.16, p-trend = 0.63), and 1.06 (95% CI 0.86-1.30, p-trend = 0.59) for overall PDI, hPDI, and uPDI respectively. Therefore, this study found no association between any plant-based diet and CVD or all-cause mortality, for an African American cohort.
1. For women without Polycystic Ovarian Syndrome (PCOS) undergoing in-vitro fertilization (IVF), there were no differences in clinical pregnancy, live birth, and miscarriage rates among patients with hyperinsulinemia (HI) or insulin resistance (IR) compared to those without.
2. Non-PCOS women with HI and IR, compared to those without, had lower basal levels of progesterone, luteinizing hormone, follicle-stimulating hormone, and estradiol, but no differences in Anti-Mullerian hormone and basal prolactin.
3. Non-PCOS women undergoing IVF with HI and IR, compared to those without, had a longer duration of ovarian stimulation, higher total gonadotropin dose, and lower peak estradiol levels.
Evidence Rating Level: 2 (Good)
Hyperinsulinemia (HI) and insulin resistance (IR) are associated with worse fertility and reproductive outcomes for women with polycystic ovarian syndrome (PCOS), with IR being a risk factor for spontaneous abortion in PCOS patients using assisted reproduction technology (ART). These worse outcomes may stem from insulin signalling being a regulator for ovulation and granulosa cell differentiation, with IR increasing apoptosis of granulosa cells and decreasing steroid hormone synthesis. However, there is little evidence on the effects of HI and IR on reproductive outcomes for non-PCOS patients using ART. Therefore, this retrospective cohort study based in China examined how HI and IR may be associated with endocrine and reproductive outcomes in non-PCOS women on their first in-vitro fertilization (IVF) cycle. The study population consisted of 1,104 women between the ages of 18 and 45, with a mean age of 31.2±4.2 years. Endocrine outcomes included hormonal level measurements. The reproductive outcomes measured were live birth (a viable delivery after 28 gestational weeks), clinical pregnancy as seen on ultrasound, and miscarriage (loss of pregnancy before 28 weeks). Overall, 40.0% had clinical pregnancy, 26.2% had live births, and 34.4% experienced miscarriages. the results found that patients with HI and IR had lower basal levels of progesterone, luteinizing hormone, estradiol, and follicle-stimulating hormone, but no differences in Anti-Mullerian hormone or basal prolactin. As well, HI and IR patients had a longer duration of stimulation significantly higher gonadotropin dose, and a lower estradiol peak compared to patients without HI and IR. However, reproductive outcomes were not significantly different. When comparing HI versus non-HI patients, 46.2% versus 39.4% had clinical pregnancy (p=0.161), 28.7% versus 23.3% had live birth (p=0.732), and 24.6% versus 27.9% had a miscarriage (p=0.670). When comparing IR versus non-IR patients, 43.6% versus 39.3% had clinical pregnancy (p=0.121), 27.8% versus 23.2% had live birth (p=0.681), and 23.3% versus 28.2% had a miscarriage (p=0.678). In conclusion, there were no differences in pregnancy outcomes for non-PCOS patients undergoing IVF with HI or IR compared to those without.
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.