2 Minute Medicine Rewind May 24, 2021
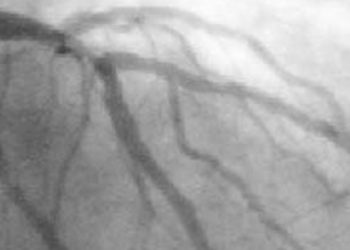
Risk factors for acute kidney injury and mortality in high risk patients undergoing cardiac surgery
1. In a retrospective cohort study, several pre-operative and operative factors were found to be associated with acute kidney injury and future mortality.
Evidence Rating Level: 2 (Good)
Acute kidney injury (AKI) is a significant cause of morality amongst hospitalized patients, especially those undergoing cardiac surgery (CS). This study sought to evaluate the predictors of the onset of AKI in CS patients, as well as the role of cardiorenal markers on predicting individual prognosis overtime. It enrolled 160 patients (mean [SD] age = 51.2 (9.7), 74.7% male) from the CS unit at Magna Graecia University of Catanzaro (Italy). Patient demographics and preoperative data such as comorbidities, blood pressure, body mass index were collected. In this cohort, AKI occurred in 58 patients (34.2%) who were characterized by statistically younger age (mean age [SD] = 48.9 [8.1] vs. 52.3 [10.4], p = 0.040). Additionally, patients with an AKI had a lower pre-operative eGFR (mean eGFR [SD] = 63.5 [23.5] vs. 76.8 [21.4], p < 0.001). The study found that AKI was associated with higher extracorporeal circulation (ECC) and cross-clamp times (p = 0.036 and p = 0.053, respectively). After the operation, a higher percentage of patients in the AKI group required a blood transfusion (87.0% vs. 66.4%, p = 0.005). Additionally, a diagnosis of AKI was associated with a median of 3 day longer stay in the hospital (p = 0.001). The study did not find any differences in rates of sepsis, atrial fibrillation, and requirement of intra-arterial balloon pump between the two groups. The risk of AKI was found to vary by type of procedure with an odds ratio of 2.19 (95% CI: 1.07 – 4.47) when comparing patients who underwent valve, aortic, and combined surgery versus those who underwent an isolated coronary artery bypass grafting (CABG). The study found that a one unit decrease in blood pH was associated with a higher risk of developing an AKI (OR = 2.20, 05% CI: 1.22 – 3.97). Finally, the presence of hypoglycemia was determined to be a strong and significant predictor of an AKI (OR = 2.55, 95% CI: 1.06 – 6.15). Overall, this is one of few studies examining risk factors associated with higher rates of AKI, thus providing crucial insight to clinicians regarding a common problem. However, the smaller sample size limits the generalizability of this study and future research should focus on further examining the identified risk factors.
Fortification of breast milk with preterm formula powder vs human milk fortifier in preterm neonates
1. Among a group of very low birth weight (VLBW) neonates, fortification with preterm formula was not found to be inferior to fortification with human milk fortifiers.
Evidence Rating Level: 1 (Excellent)
Fortification of expressed breast milk (EBM) with human milk fortifiers (HMF) has been shown to lead to increased weight and length in VLBW neonates. However, its use is limited due to high cost and risk of feed intolerance. In this parallel group, non-inferiority randomized trial, researchers sought to investigate whether or not fortification with preterm formula (PTF) would be noninferior to HMF and provide a potentially cheaper alternative for fortification. The primary outcome measured to assess this was the rate of in-hospital weight gain. The secondary outcomes measured were mortality, rate of increase in head circumference and length at discharge, feed intolerance, necrotizing enterocolitis, intraventricular hemorrhage (IVH), metabolic bone disease (MBD), anemia requiring transfusion, late metabolic acidosis (LMA), bronchopulmonary dysplasia (BPD), and retinopathy of prematurity (ROP). The study randomized 123 neonates, born at 34 weeks or less, into a control group which received HMF (n = 63) and an intervention group which received PTF (n = 60). Baseline characteristics of the neonates such as birth weight and gestation were comparable between the two groups. The mean (SD) weight gain in neonates receiving PTF was 15.7 (3.9) g/kg/day while neonates receiving HMF gained 16.3 (4) g/kg/day (mean difference = -0.5g/kg/day, 95% CI: -1.9 to 0.7). This did not cross a pre-specified inferiority margin of 2g/kg/day. Similarly, the gain in length and head circumference was comparable in both groups. The incidence of feed intolerance was lower in the PTF group (incidence rate ratio [IRR] = 0.29, 95% CI: 0.04 to 0.95). The proportion of patients in whom fortification had to be withheld for 24 or more hours was lower in the PTF group (5% vs 22%, risk ratio = 0.22, 95% CI: 0.07 – 0.75). There were no significant differences between the groups in terms of incidence of NEC, mortality, sepsis, MBD, IVH, PDA, ROP or BPD. Thus, the study concluded that PTF is non-inferior to HMF when used in VLBW neonates. With further validation, this may provide a more cost-friendly alternative to HMF for EBM fortification, especially for areas and individuals who may have limited financial resources.
Risk of clinical sequelae after the acute phase of SARS-CoV-2 infection: retrospective cohort study
1. Among a large cohort from United States, infection with SARS-CoV-2 led to excess risk of developing new clinical sequelae, less commonly seen in other viral illnesses, after the acute phase of the infection.
Evidence Rating Level: 2 (Good)
In addition to the acute threat to life that the SARS-CoV-2 infection can pose to an infected individual, there is emerging literature suggesting that infection is additionally associated with significant long-term sequelae that can contribute to increased morbidity and mortality worldwide. In this retrospective cohort study, researchers examined individuals aged 18 to 65, enrolled continuously in a health plan in 2019 – 2020, who were diagnosed with COVID-19 to further investigate the emergence of clinical sequalae following the acute phase of infection. The study utilized two control groups. The first comparator group were individuals aged 18 to 65, enrolled in a continuous health plan in 2019 or 2020, who were not diagnosed with COVID-19. There were 226 586 matched pairs made with this comparison group. The other comparator group included individuals aged 18 to 65, enrolled in a continuous health program in 2016, 2017 or 2018, who developed a viral-respiratory tract illness. The study matched 244 276 pairs with this comparison group. Examples of various sequelae included arrythmias, dermatitis, stroke, cardiomyopathy, hypercoagulability/deep vein thrombosis, kidney injury, seizures, and many more. All three comparator groups had lower rates of clinical sequelae develop, although the difference was smallest when compared to the viral lower respiratory tract group. The study found that 10.01% of individuals with COVID-19 developed new sequela after the acute phase of the infection and 4.01% had more than one type of sequelae. In the 2020 group, 7.08% of patients developed a clinical sequela (difference = 2.93%, p < 0.01) and 1.99% developed more than one type of sequelae (difference = 2.02%, p < 0.01). The 2019 group demonstrated that 7.36% of patients developed a clinical sequela (difference = 2.68%, p < 0.01) and 2.11% developed more than one sequela (difference = 1.91%, p < 0.01). In the viral lower respiratory tract matched groups, 10.38% of individuals with COVID-19 developed one sequela compared to 9.71% of those with another viral illness (difference = 0.68%, p < 0.01). 4.22% of individuals with COVID-19 developed more than one sequela compared to 3.25% of individuals with another viral illness (difference = 0.97%, p < 0.01). Finally, the study concluded that excess risk for developing clinical sequelae increased significantly with age. Several studies in the past have examined acute sequelae associated with COVID-19, however, this is one of the first large scale studies focusing on sequelae after the acute infection. The significant risk of sequelae development reported in the study provides valuable insight into the ongoing impact COVID-19 can have on a patient’s medical course, and is highly relevant for healthcare planning discussions.
Association of NO2 and other air pollution exposures with the risk of Parkinson disease
1. Among a cohort of individuals from South Korea, exposure to nitrogen dioxide (NO2) was found to be associated with an increased risk of developing Parkinson’s disease (PD).
Evidence Rating Level: 2 (Good)
Increased air pollution levels have been identified to be associated with neurodegenerative changes in recent studies. This retrospective cohort study aimed to determine the association between incidence of PD and six types of air pollutants (nitrogen dioxide [NO2], sulfur dioxide [SO2], carbon monoxide [CO], and particulate matters [PM2.5 and PM10]). It enrolled 78 830 adults older than 40 years (mean age [SD] = 54.4 [10.7], 52.1% were female) without PD from different districts. The study collected data on air pollutant levels from the different districts in which the participants resided. Each participant was followed up with annually for 9 years to determine if a new diagnosis of PD had been made. The study also collected data on other covariates such as age, sex, pre-existing comorbidities, and type of health insurance. The study found that exposure to NO2 was associated with an increase in risk of PD (hazard ratio for highest vs. lowest quartile, 1.34; 95% CI, 1.02 – 1.95, p = 0.045). The association was present after adjusting for demographic factors and comorbidities. In comparison, there was no association found between levels of SO2, CO, PM2.5, PM10 and incidence of PD, for both adjusted and non-adjusted analysis. The study demonstrated that the hazard ratios for incident PD according to NO2 exposure showed a statistically significant increase when NO2 levels were greater than 0.038 parts per million. One of the studies largest limitation was not adjusting for factors such as socioeconomic status, occupation, and workplace exposures. However, this is still one of few large-scale studies evaluating the link between air pollutants and incident PD. Given the study’s findings, future studies in this area are encouraged and required to make further informed public health policies.
1. Among a group of primary school children in Tanzania, a combination intervention aimed at enhancing handwashing had no effect on soil-transmitted helminth infection.
Evidence Rating Level: 1 (Excellent)
Soiled-transmitted helminth (STH) infections are frequent amongst school children in low- and middle-income countries. It represents significant morbidity as it is associated with increased rates of anemia and impaired physical and cognitive development. The aim of the randomised controlled trial was to evaluate the effectiveness of a specialized program in reducing the incidence of these infections. The intervention involved 3 components: health education for children, engagement meeting with parents, and slight modification of the school environment to facilitate handwashing. The trial enrolled 16 primary schools, 8 of which were allocated to the intervention group (n = 4872 students), while the rest were given standard health education (n = 4607 students). The two groups were balanced in terms of sex and students’ age. The study found that 72% of students from the intervention group reported using soap and water to wash their hands at school compared to 39% of students in the control group (adjusted odd’s ratio [aOR] = 3.7, 95% CI = 1.35 to 10.15, p = 0.002). In comparison, 45% of children in the intervention group reported washing their hands with soap and water at home versus 33% of children from the control group (aOR = 1.02, 95% CI = 0.74 to 1.39, p = 0.90). The combined prevalence of Ascaris lumbricoides and Trichuris trichiura infection was 39% in both groups (aOR = 1.19, 95% CI 0.74 to 1.91). Thus, the study concluded that the intervention had a significant effect on improving handwashing amongst children at school. However, there was no difference noted between the groups in terms of handwashing at home. The study predicted that this was likely the primary reason for a lack of difference in infection rates amongst the group, along with other possibilities such as contaminated food and water. Therefore, it provides direction for future studies to focus on evaluating the effectiveness of these factors to reduce infection rates.
Image: PD
©2021 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.