2 Minute Medicine Rewind November 22, 2021
Association of social support with functional outcomes in older adults who live alone
1. Identifiable support buffered the risk of prolonged nursing home stays for older adults facing a new health stressor while living alone
Evidence Rating Level: 2 (Good)
Older adults who live alone are at risk for poor health outcomes. It is unclear whether social support helps mitigate the risk of living alone, especially during periods of sudden health changes, among this population. To assess the association between social support and functional outcomes in older adults who live alone, this longitudinal prospective cohort study recruited 4772 community-dwelling older adults, 65 years or older, who lived alone and independently between March 2006 and April 2015. Participants were followed up biennially through April 2018 and information on identifiable support (i.e., can the participant identify a relative/friend who could help with personal care if needed), health shock (i.e., new diagnosis of cancer/stoke/heart attack, hospitalization), and interaction (multiplicative and additive) was obtained. The primary outcome measures were activities of daily living (ADL) dependency, prolonged nursing home stay (≥30 days), and death. At baseline, of 4772 older adults who lived alone (median [IQR] age, 73 [68-81] years; 3398 [71%] women), 1813 (38%) could not identify support. During the study, 3013 (63%) participants experienced a health shock. In the presence of a health shock, support was associated with a lower risk of a prolonged nursing home stay (predicted probability over 2 years, 14.2% vs 10.9%; P = .002). This association was not observed when a health shock was absent (predicted probability over 2 years, 1.9% vs 1.4%; P = .21). Support was not associated with incident ADL dependence or death. It can be concluded that identifiable support may buffer the risk of prolonged nursing home stays for older adults facing a new health stressor while living alone.
Factors associated with consent for organ donation: A retrospective population-based study
1. A modifiable factor independently associated with positive consent was a collaborative approach by a physician and donation coordinator
2. A modifiable factor independently associated with negative consent included a telephone approach for consent
3. The most common reason substitute decision-makers were not approached for consent was a late referral by the health care team
Evidence Rating Level: 2 (Good)
In Canada, demand for organs outstrips supply. Despite public support for organ donation, donation rates vary considerably by region. Even in jurisdictions with donation consent registries or opt-out consent systems, substitute decision-makers play an important role in the organ donation process and their consent rates vary widely. Consequently, it is possible that the process of obtaining consent has a substantial impact on the decision to donate. This retrospective cohort study aimed to identify modifiable approach- and system-level factors that may positively influence a substitute decision-maker’s decision to consent for organ donation in Ontario, Canada. Demographics, patient clinical data, data on substitute decision-makers, and donation consent approach characteristics for all adults (≥18 years) referred for organ donation in Ontario between April 2013 and June 2019 were obtained and analyzed. Study outcomes were consent for organ donation and approach rate. A total of 34 837 referrals for organ donation were identified. 6548 (18.8%) substitute decision-makers were approached for consent. Of these, 3927 (60% of approaches) consented for organ donation and 1883 (48% of consents) proceeded to be organ donors. A modifiable factor independently associated with positive consent was a collaborative approach by a physician and donation coordinator (adjusted OR 1.26, 95% CI 1.01–1.59). A modifiable factor independently associated with negative consent included a telephone approach for consent (adjusted odds ratio [OR] 0.46, 95% confidence interval [CI] 0.35–0.58). The most common reason substitute decision-makers were not approached for consent was a late referral by the health care team (45.2%). To improve organ donation rates, interventions should increase physician participation in the approach process, prioritize in-person consent approaches, and ensure timely referrals to organ donation organizations.
1. For patients in ST-elevation myocardial infarction, administration of aspirin 10 minutes prior to nitroglycerin led to greater pain reduction compared to simultaneous administration.
2. Patients receiving aspirin prior to nitroglycerin additionally required fewer additional doses of nitroglycerin and were less likely to require opioids for pain control.
Evidence Rating Level: 2 (Good)
Acute coronary syndrome (ACS) describes a range of conditions associated with sudden, reduced blood flow to the heart, including unstable angina, non-ST elevation myocardial infarction (NSTEMI), and ST-elevation myocardial infarction (STEMI). ACS is a cause of significant morbidity and mortality worldwide and early treatment is critical for reducing negative health outcomes. Current guidelines from the American College of Cardiology (ACC) and the American Heart Association (AHA) state that aspirin and nitroglycerin should be administered to patients with ACS. However, the order or timing of giving these medications is not recognized. This retrospective cohort study aimed to examine if there was any benefit to giving aspirin before or after nitroglycerin in cases of ACS. A total of 2594 patients with ACS who received aspirin plus nitroglycerin in prehospital settings were identified using the National Emergency Medical Services Information System (NEMSIS) database. The patients were separated into 2 groups based on which medication was administered first: an aspirin-first group and a nitroglycerin-first group. The 2246 patients in the aspirin-first group were further stratified based on the time between administration of aspirin and the first dose of nitroglycerin. The 348 patients in the nitroglycerin-first group were stratified in a similar way. The outcome measures included administration of additional doses of nitroglycerin following the first dose and the subjective feelings of the patients. It was found that in patients with STEMI ischemia, administering aspirin 10 minutes before nitroglycerin led to a >20% reduction in need for additional nitroglycerin, a >7% decrease in subjective pain experience, and a reduced need for additional opioids, compared with administering them simultaneously. Additionally, the aspirin-first group in total experienced a 39.6% decrease in subjective pain experience after giving additional nitroglycerin compared with the nitroglycerin-first group. Study results may have implications for how initial management is carried out for patients with ACS.
1. The rate of initiation of injection drug use among individuals who received chronic prescription opioid treatment for non-cancer pain was 8.4 times higher than among opioid nave individuals
Evidence Rating Level: 2 (Good)
Injection drug use (IDU) is a progressively increasing practice associated with substantial morbidity and mortality. Although prescription opioids are not recommended as first-line treatment of chronic non-cancer pain, adequate non-opioid alternatives are not always available or accessible. It has been hypothesized that patients medically prescribed opioids for pain may be at higher risk of initiating IDU. This retrospective cohort study examined the association between prescription opioid treatment for non-cancer pain and subsequent initiation of IDU among individuals without a history of substance use at baseline. The Integrated Data and Evaluative Analytics (IDEAs) cohort, composed of all reported cases of hepatitis B and tuberculosis and all individuals tested for hepatitis C and HIV at the British Columbia Centre for Disease Control Public Health Laboratory between 1992 and 2015, was used. Episodes of prescription opioid use for non-cancer pain were identified based on drugs dispensed between 2000 and 2015. Episodes were classified by increasing length and intensity of opioid use. Individuals with a chronic episode (lasting ≥90 episode days; with ≥90 days’ drug supply and ≥50% episode intensity) were matched 1:1:1:1 on socioeconomic variables to those with episodic (lasting ≥90 days; with <90 days’ drug supply and/or <50% episode intensity) or acute (lasting <90 days) episodes and to those who were opioid naïve. IDU initiation was identified using a validated administrative algorithm. A total of 59 804 participants (14 951 in each opioid use category) were included and followed for a median of 5.8 years. 1149 participants initiated IDU. Cumulative probability of IDU initiation was found to be highest for participants with chronic opioid use (4%), followed by those with episodic use (1.3%), acute use (0.7%), and those who were opioid naïve (0.4%). Risk of IDU initiation was 8.4 times higher for those with chronic opioid use versus those who were opioid naïve (90% CI 6.4 to 10.9). Initiation of IDU was more frequent at higher opioid doses and younger ages. These findings may have implications for strategies to prevent IDU initiation.
1. Calcification deposits with a diameter of 6 mm or more in patients younger than 56 years of age were associated with shoulder pain.
2. A distance from calcification to tendon insertion of 6 mm or more in patients 56 years of age and older was associated with pain.
3. A signal on Colour Doppler was associated with shoulder pain.
Evidence Rating Level: 3 (Average)
The shoulder is a common anatomical site for musculoskeletal (MSK) pain. Previous research has shown that calcifications and pain are associated. Calcification size is relevant and shoulders with radiologically-detected calcific deposits >1.5 cm in length are more likely to be symptomatic. Ultrasound (US) is considered to be reliable in the detection and localization of calcifications associated with MSK pain. This case-control study aimed to further investigate US features associated with the presence of shoulder complaints. A total of 140 cases, aged 18-70 years, suffering from shoulder pain and referred for unilateral shoulder US were recruited between February 2018 and June 2020. Controls were invited on a voluntary basis and 62 were randomly selected. Results showed that a calcification size ≥6 mm when age <56 (p = 0.02) and a distance to tendon insertion ≥6 mm when age ≥56 (p = 0.009) were features on US only seen in symptomatic shoulders. Additionally, positive signal on Colour Doppler was more frequent in symptomatic participants (26/140 vs. 2/62, p = 0.003). The US criteria highlighted in this study may aid diagnosis when symptoms and physical examination are ambiguous.
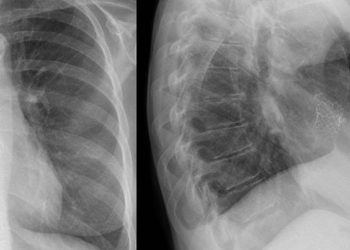
Image: PD
©2021 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.



![2 Minute Medicine: Pharma Roundup: Price Hikes, Breakthrough Approvals, Legal Showdowns, Biotech Expansion, and Europe’s Pricing Debate [May 12nd, 2025]](https://www.2minutemedicine.com/wp-content/uploads/2025/05/ChatGPT-Image-May-12-2025-at-10_22_23-AM-350x250.png)


