Comparable outcomes suggested across antibiotic spectrum for pediatric CAP
Image: PD
1. Despite 2011 national clinical practice guidelines suggesting narrow-spectrum antibiotics as empiric therapy for children hospitalized with presumed community-acquired pneumonia (CAP), approximately only 10% of children are treated accordingly.
2. This study suggests no significant differences in length of stay, admissions to ICU, readmissions, or costs between children treated with narrow- vs. broad-spectrum antibiotics for pediatric CAP.
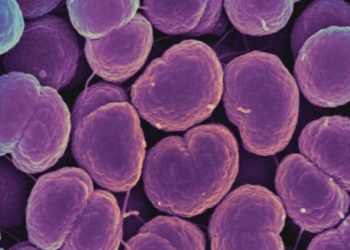
Study Rundown: Over 150,000 children are hospitalized annually with community acquired pneumonia (CAP). These children are most often treated with empiric antibiotics before a causative organism is identified. The Pediatric Infectious Diseases Society and Infectious Diseases Society of America collaborated in 2011 to release clinical practice guidelines for the choice of empiric antibiotics for children over 3 months of age with presumed CAP. These guidelines suggest empiric coverage with either penicillin or ampicillin, which are narrow-spectrum antibiotics known to adequately cover Streptococcus pneumoniae, the most common causative pediatric CAP organism. Despite these guidelines, research indicates that approximately only 10% of children hospitalized for CAP are treated appropriately. This observational study compared clinical and cost outcomes in children hospitalized for CAP receiving either narrow- or broad-spectrum antibiotics. Researchers found no significant difference in median length of stay (LOS), number of admissions to the ICU, readmissions, or costs between the 2 groups. Though limited by its design, this study provides additional evidence in favor of the 2011 guidelines, and suggests judicious antibiotic usage for pediatric CAP to promote proper antibiotic stewardship.
Click to read the study published today in Pediatrics
In-Depth [observational study]: This study examined 149 853 children aged 6 months to 18 years with an ICD-9 code for CAP at 43 freestanding, tertiary care children’s hospitals from the Pediatric Health Information System database. Children with complex chronic conditions, transfers from another hospitals, or previous hospitalization within 30 days were excluded for concern for healthcare-associated pneumonia. Additionally, children with low severity of disease (LOS < 2 days) and high severity (requiring pleural drainage, admission to ICU, mechanical ventilation, or death within first 2 days of hospitalization) were excluded. After exclusion, 13 954 (89.7%) children treated with broad-spectrum antibiotics (ceftriaxone, cefotaxime) and 1 610 (10.3%) treated with narrow-spectrum antibiotics (penicillin, ampicillin) were examined. No significant differences were found in admissions to ICU (1.1% broad v. 0.8% narrow, adjusted odds ratio: 0.85, 95% CI: 0.27 – 2.73) or readmissions (2.3% broad v. 2.4% narrow, adjusted odds ratio 0.85, 95% CI: 0.45 – 1.63). There was also no significant difference in LOS for the 2 groups(adjusted difference: 0.12 days, 95% CI: -0.02 – 0.26) or cost of hospitalization (adjusted difference: -$14.4, 95% CI: -$177.1 – $148.3).
By Neha Joshi and Leah H. Carr
More from this author: Dexamethasone efficacy suggested in high-risk infants with bronchiolitis, Antepartum and intrapartum events both linked to neonatal HIE, Adult decision rules poor proxy for diagnosing pediatric PE, Pediatric readmissions likely a poor proxy for hospital quality, Quality improvement methods increase adherence to pediatric UTI guidelines
© 2013 2minutemedicine.com. All rights reserved. No works may be reproduced without expressed written consent from 2minutemedicine.com. Disclaimer: We present factual information directly from peer reviewed medical journals. No post should be construed as medical advice and is not intended as such by the authors, editors, staff or by 2minutemedicine.com. PLEASE SEE A HEALTHCARE PROVIDER IN YOUR AREA IF YOU SEEK MEDICAL ADVICE OF ANY SORT.