Cranial radiotherapy associated with increased risk of anterior hypopituitarism
1. In a retrospective review of over 700 childhood cancer survivors (CCS) treated with cranial radiotherapy, over 50% developed anterior pituitary dysfunction.
2. A significant number of CCS who developed growth hormone and sex-hormone deficiencies were not recognized, leading to serious cardiovascular and musculoskeletal morbidities.
Evidence Rating Level: 3 (Average)
Study Rundown: Anterior hypopituitarism is a known complication of cranial radiotherapy (CRT) for childhood malignancies. The risk of anterior pituitary dysfunction in childhood cancer survivors (CCS) increases in a time-dependent fashion and patients with unrecognized deficiencies may demonstrate significant morbidity in adulthood. The purpose of this study is to describe the long-term health outcomes and complications of this patient population. The authors retrospectively analyzed over 700 patients treated with CRT. After an average follow-up of 27.3 years, the authors found that over 50% of patients had at least one anterior pituitary deficiency with growth hormone deficiency (GHD) and luteinizing/follicular stimulating hormone deficiency (LH/FSHD) being the most common. Furthermore, the majority of individuals with GHD and LH/FSHD did not receive replacement hormone therapy, which led to significantly increased complications including decreased muscle mass and exercise tolerance, hypertension, dyslipidemia, and low bone mineral index compared to a reference population. Risk factors for the development of anterior hypopituitarism included male sex, obesity, white race, and increasing doses of radiation. This is the largest patient cohort following the development of anterior pituitary complications in CCS and the results of this trial support the hypothesis of lifetime screening for this patient population. The main limitation of this trial is the retrospective study design and the use of static endocrine testing sectional data.
Click to read the study in JCO
Relevant Reading: Hypothalamic-pituitary dysfunction after radiation for brain tumors
In-Depth [retrospective cohort]: The authors performed a retrospective study of a long-term cohort of childhood cancer survivors from the St. Jude Lifetime Cohort (SJLIFE) study. A total of 748 patients (mean age: 27.3 years; range: 10.8 to 47.7 years) who had undergone CRT were observed for a mean duration of 27.3 years (range 10.8 to 47.7 years). Overall, 51.4% (n=371) patients had one of four anterior pituitary deficiencies; 46.5% (n=348) of patients had growth hormone deficiency (GHD), 10.8% (n=79) had luteinizing hormone/follicular stimulating hormone deficiency (LH/FSHD), 7.5% (n=56) with thyroid stimulating hormone deficiency (TSHD), and 4% (n=29) with ACTH deficiency. Only 1 (0.3%) individual with GHD and 17 (21.5%) patients with LH/FSHD were receiving hormone replacement therapy. Untreated GHD was associated with decreased muscle mass and exercise tolerance, while untreated LH/FSHD was associated with hypertension, dyslipidemia, low bone mineral density and slow walking. Male sex and obesity were associated with LH/FSHD, and white race with LH/FSHD and TSHD. CRT doses of 22-29.9 Gy were associated with GHD compared to doses less than 22 Gy, and doses >30 Gy were associated with TSHD and ACTHD.
More from this author: Rituximab linked with reduced chronic immune disease following stem cell transplantation, High-dose prophylaxis for hemophilia increases costs with minimal benefit, Ambrisentan found ineffective against idiopathic pulmonary fibrosis
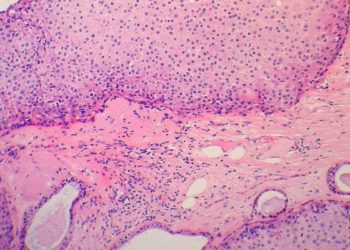
Image: PD
©2014 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. No article should be construed as medical advice and is not intended as such by the authors, editors, staff or by 2 Minute Medicine, Inc.