Early mobilization after ICU mechanical ventilation does not improve survival
1. Early mobilization of patients after mechanical ventilation in the intensive care unit (ICU) did not result in an improvement in the number of days alive and out of the hospital.
2. Early mobilization was associated with more adverse events than routine care.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Patients with a critical illness are often admitted to the ICU, many of whom develop weakness, resulting in increased mortality and prolonged recovery course. This weakness is especially marked in mechanically ventilated patients, due to muscle wasting and co-morbidities from their critical illnesses. Early mobilization has been suggested to mitigate the impact of ICU-associated weakness, although with limited evidence and regimen standards. The current study was a randomized controlled trial to evaluate the effects of early mobilization or usual care on the recovery of patients who underwent mechanical ventilation in the ICU. By 180 days, the number of days patients were alive and out of the hospital was not significantly different between the two groups. Both groups also showed similar outcomes in quality of life and function. Early mobilization was associated with a higher rate of adverse events. It was noted that patients receiving usual care had a higher level of baseline mobilization than in previous cohort studies. Nevertheless, these results demonstrated that early mechanical ventilation does not impact the number of days alive and out of the hospital compared to usual care.
Click here to read the study in NEJM
In-Depth [randomized controlled trial]: This study was a multicenter, randomized controlled trial assessing the impact of early mobilization on patients who underwent mechanical ventilation in the ICU. Adult patients were eligible if they were expected to receive mechanical ventilation after randomization and were stable enough for mobilization. Exclusion criteria included rest-in-bed orders, dependency in activities of daily living prior to admission, and brain or spinal injury. Overall, 750 adult patients were randomized 1:1 to receive either early mobilization (via sedation minimization and daily physiotherapy) or usual care (baseline mobilization provided in the ICU). The primary outcome was the number of days patients were alive and out of the hospital at 180 days following randomization. The early-mobilization group had significantly more mobilization time daily than the usual-care group, and patients receiving early mobilization were able to stand earlier than those receiving usual care. The median number of days alive and out of the hospital was 143 (interquartile range [IQR], 21 to 161) in the early-mobilization group and 145 days (IQR, 51 to 164) in the usual-care group (absolute difference, -2.0 days; 95% Confidence Interval [CI], -10 to 6; p=0.62). The mortality rate was 22.5% for the early-mobilization group and 19.5% for the usual-care group (odds ratio, 1.15; 95% CI, 0.81 to 1.65). Notably, adverse events attributable to mobilization, such as arrhythmias, blood pressure alteration, and desaturation, were more prevalent in the early-mobilization group (9.2%) than in the usual-care group (4.1%) (p=0.005). Although the level of mobilization given under usual care was higher than in cohort studies, this was consistent with international guidelines and other clinical trials. These results showed that early mobilization did not impact the number of days alive and out of the hospital among patients receiving mechanical ventilation in the ICU.
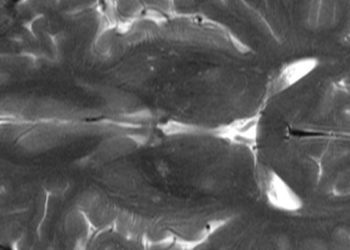
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.