Incidence, risk factors, and in-hospital mortality of post-operative AKI following aortic dissection repair
1. For patients undergoing surgical interventions for acute type A aortic dissections (AAAD), post-operative acute kidney injury was shown to increase patient mortality risk.
2. Risk factors associated with AKI occurrence included high BMI, chronic kidney disease, chronic liver disease, cardiopulmonary bypass duration, RBC transfusion, and hypoproteinemia.
3. Risk factors associated with in-hospital mortality for patients with AKI included AKI stage, lactic acidosis, CRRT, and deep hypothermic circulatory arrest.
Evidence Rating Level: 2 (Good)
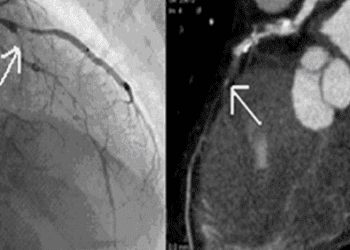
Acute kidney injury (AKI) is a common complication after cardiac surgery. Particularly following surgical treatment for acute type A aortic dissections (AAAD), a life-threatening cardiac condition, AKIs occur at an incidence rate ranging from 20.2% to 66.7%. The variance in rate is partly due to the lack of a uniform definition of AKI. This study seeks to identify the incidence rate of AKI by the 2012 Kidney Disease Improving Global Outcomes Acute Injury (KDIGO) Work Group criteria, as well as to identify risk factors and in-hospital mortality for AKIs, after surgical interventions for AAAD. This retrospective cohort study included 335 patients with AAAD who underwent surgery while in hypothermic circulatory arrest at West China Hospital of Sichuan University. Of these patients, 71.944% experienced an AKI. By severity, 35.26% had AKI stage 1, 31.95% had AKI stage 2, and 32.78% had stage 3 AKI. After screening their medical records, risk factors found to be associated with AKI occurrence include body mass index (OR, 1.221), chronic kidney disease (OR, 12.352), chronic liver disease (OR, 2.207), cardiopulmonary bypass duration (OR, 1.008), red blood cell transfusion (OR, 1.186), and hypoproteinemia (OR, 5.091). In-hospital mortality for patients who experienced post-surgical AKIs was 21.16%. Risk factors associated for in-hospital mortality for patients who experienced AKI include AKI stage (OR, 3.322), deep hypothermic circulatory arrest (OR, 2.586), lactic acidosis (OR, 3.407) and continuous renal replacement therapy (OR, 3.156). Limitations to this study include that baseline serum creatinine may have only been taken post-AAAD in some patients which can affect the incidence of AKI. This study demonstrates that a significant portion of patients undergoing surgery for AAAD experience AKIs, which come with considerable mortality. It also provides insight into factors that may increase risk of AKI and its associated mortality. Further studies should seek factors which improve post-operative outcomes for AAAD patients by accounting for these AKI-associated risk factors, in a multicentre format.
Image: PD
©2020 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.