Ozanimod can inhibit immune system response and improve ulcerative colitis symptoms
1. Patients receiving 1mg of the lymphocyte-suppressing agent Ozanimod showed significant clinical improvement in ulcerative colitis (UC) symptoms compared to placebo at 8 weeks and 32 weeks after treatment was started.
2. Absolute blood lymphocyte counts were reduced in patients taking 0.5mg and 1mg doses of Ozanimod at 8 weeks, by 32% and 49% respectively, though no significant differences in adverse side effects were observed compared to the placebo group.
Evidence Rating Level: 1 (Excellent)
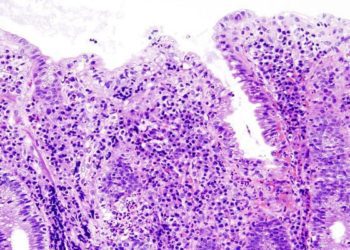
Study Rundown: UC is an inflammatory disease of the colon strongly mediated by lymphocytic cells. Modern treatments therefore have aimed to modulate immune system response, and finding better oral treatments has been a consistent goal. Sphingosine-1-phosphate (S1P) receptors 1-5 are expressed on lymphocytic cells, and agonist activation of them results in receptor internalization inhibiting lymphocytes from leaving secondary lymphoid tissue. A phase 2 study evaluating the S1P1 and S1P5 agonist Ozanimod showed reduction in circulating lymphocytes and inflammation for multiple sclerosis patients, and this study aimed to evaluate the effects of Ozanimod in those with UC.
The primary outcome measured in the study was clinical remission, and those on 1mg of Ozanimod showed significant symptom remission at weeks 8 and 32 of the study compared to the placebo group. Secondary outcomes of clinical response, mucosal healing, and histologic remission all showed patients receiving either 0.5mg or 1mg had improved outcomes relative to the placebo group. Immunologically, at 8 weeks patients on both dosing groups had significantly reduced circulating lymphocyte counts. Patients on Ozanimod did not have substantial differences in adverse outcomes compared to those in the placebo group. The study findings may indicate better treatment efficiency as treatment persists, though the length and size of the study may not have been long enough to optimally elicit information about safety and risk of adverse effects.
Click to read the study in NEJM
Relevant Reading: Ozanimod (RPC1063) is a potent sphingosine-1-phosphate receptor-1 (S1P1) and receptor-5 (S1P5) agonist with autoimmune disease-modifying activity
In-Depth [randomized controlled trial]: This was a double blind phase 2 trial conducted from 2012-2015 at 57 centers internationally. UC patients ages 18-75 with a Mayo score (index to assess severity of presentation, higher scores being worse presentation) of 6-12, with the endoscopic score component of 2-3, were eligible for the study (n=199). Random assignments of patients to placebo, 0.5mg, or 1mg Ozanimod groups was done in a 1:1:1 ratio, with stratification for prior exposure to TNF antagonists. Dose escalation was done for 1 week and then maintained until week 8, at which point those with no clinical response were allowed to switch to open-label treatment. Assessments of various types were done at baseline and weeks 4, 8, 20, and 32. The primary outcomes was clinical remission (Mayo Clinic score ≤2, with no subscore >1), secondary outcomes were clinical response (Mayo score reduction of ≥3 points and ≥30% from baseline, and decrease in the rectal bleeding subscore of ≥1 point or a subscore of ≤1), Mayo score change from baseline, and mucosal healing (endoscopy subscore ≤1). Other exploratory outcomes and adverse effects were also measured. Clinical remission was statistically significant at week 8 between the 1mg and placebo groups (16% vs. 6%, p=0.048) but not between the 0.5mg and placebo group (14% and 6%, p=0.14). At 32 weeks clinical remission was statistically significant for both the treated groups compared to placebo (21% for 1mg, 26% for 0.5mg, 6% for placebo). Secondary outcomes of clinical response (except 0.5mg vs placebo), mucosal healing, and histologic remission were all significantly better for both treated groups compared to placebo at week 32. There was no observed difference in adverse outcomes between the 3 groups.
Image: PD
©2016 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.