Patient Basics: Urinary Incontinence
Originally published by Harvard Health.
What Is It?
Urinary incontinence is a loss of control over urination. Urine leaks before you are able to get to a toilet.
There are many types of urinary incontinence.
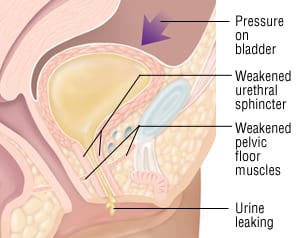
One type is stress incontinence. Your pelvic muscles are located beneath your bladder. Stress incontinence occurs when your pelvic muscles aren’t strong enough. They cannot withstand a “stress” or pressure pushing on the bladder.
When your pelvic muscles give way, they release their squeeze around the bottom of your bladder. As a result, urine can drain out.
Stress incontinence is common during:
- Pregnancy
- Coughing
- Sneezing
- Lifting
- Laughing
- Some awkward body movements
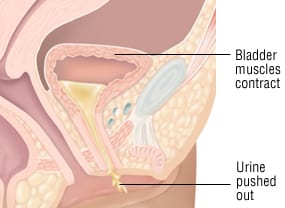
Another common type of urinary incontinence is urge incontinence. This is also called overactive bladder. The bladder is overly sensitive to stretching and nerve signals. You may feel the urge to urinate when your bladder is only partly filled. Also, your bladder can squeeze after only a minimal trigger.
Many women have urinary incontinence after childbirth. Pregnancy and childbirth can affect the conditioning of the pelvic muscles. They can also stretch and injure the pelvic nerves. Incontinence may last for a surprisingly long time after childbirth.
Temporary urinary incontinence is frequently caused by a urinary tract infection (UTI). It can also result from uterine prolapse. This is a sagging of the uterus. Irritation of the vagina (vaginitis) is another cause of temporary incontinence.
Neurologic problems such as multiple sclerosis or spinal cord injury can cause incontinence. They can cause the bladder to overfill and overflow. Or they can cause the bladder to empty unpredictably.
Incontinence can be a complication of radiation treatment or prostate surgery.
Some people have normal bladder function and control. But they are not able to move easily. This can lead to urinary incontinence because the person cannot get to the bathroom in time.
Urinary incontinence is more common in women than in men.
Symptoms
The main symptom of urinary incontinence is leakage of urine. This leakage can be frequent or rare. It can be a soaking or a small squirt.
Urge incontinence can cause leakage during sleep.
A urinary tract infection is likely to be causing incontinence if urine leakage is accompanied by:
- Pain during urination
- Pink, red or dark discoloration of your urine
- Urine odor
- Abdominal or back pain
- Frequent urinating
Diagnosis
Your doctor will review your medical history.
Your doctor may ask you to keep a voiding diary for one to three days. You should record:
- Times and amounts of urine leakage
- Fluid intake
- Possible triggers (ex. physical activity, coughing, laughing)
A neurological examination and a pelvic examination may be done. These will help to reveal the cause of your urinary incontinence.
You may also have a test to see whether you can empty your bladder completely. You will be asked to urinate to empty your bladder. Then, the amount of urine left in the bladder will be measured.
Your doctor should check for a urinary tract infection.
If your doctor suspects that nerve injury is causing your incontinence, you may need an imaging study. This may be a computed tomography (CT) scan or magnetic resonance imaging (MRI) scan of your brain or spinal cord.
Expected Duration
Urinary incontinence may be a short-term problem. This is likely if it is related to pregnancy or to a UTI.
Urinary incontinence is more often a long-term problem if it results from:
- Muscle weakness
- Pelvic injury
- Nerve problems
Prevention
Urinary incontinence is not usually prevented. Rather, the problem is treated once it begins.
Urinary incontinence is more common in women who have had a hysterectomy.
Obese women are more likely to develop urinary incontinence. So are women who don’t exercise regularly.
Treatment
Kegel Exercises
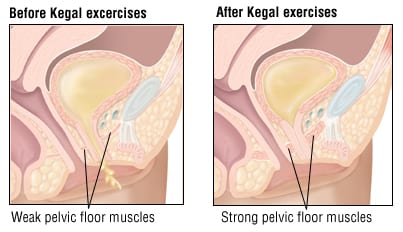
Many women can improve or eliminate urinary incontinence by doing pelvic muscle exercises. These are called Kegel exercises. They strengthen the muscles that surround the openings of the urethra, vagina and rectum.
To do Kegel exercises, squeeze your muscles to tighten your rectum and vagina. Hold Kegel squeezes for 6 to 8 seconds. Group 8 or 12 squeezes into each session. You can repeat these exercises several times each week.
Kegel exercises are particularly helpful for stress incontinence. They can also help control other types of incontinence. It can take several months or longer to see benefits.
Bladder Retraining
Urge incontinence can be improved by retraining. The goal is to help your bladder become less sensitive to its triggers over time.
The squeezing of your bladder is a conditioned response. You need to give your bladder a period of time when it is not stimulated by the signal of a full bladder. This helps your bladder to be less “jumpy.”
To accomplish this, empty your bladder on a rigid schedule before it becomes full. You may need to urinate every half hour or hour. Gradually lengthen the interval between your bathroom stops. Your bladder may not respond as urgently after several weeks of retraining.
You also can improve urge incontinence by calming your bladder signals. Try not to race to the bathroom when you feel an urge to urinate. Instead, try sitting and breathing deeply for a short time. Or do Kegel exercises to distract your bladder.
Some specialists provide bladder sphincter biofeedback. This shows levels of bladder, rectum and abdominal pressure during Kegel squeezes or during relaxation techniques.
Medications
Several medications can improve symptoms of urge incontinence. The most commonly used medicines are oxybutynin (Ditropan) and tolterodine (Detrol).
Women who have a UTI are given antibiotics.
Some post-menopausal women have vaginitis caused by too little estrogen. Estrogen creams or tablets in the vagina can be helpful. Estrogen does not help urinary incontinence in women who do not have vaginitis.
Devices to Strengthen the Pelvic Muscles
Your doctor may recommend using cone-shaped weights. You place one of these cones into your vagina before you begin pelvic muscle exercises. These maximize the muscle-conditioning effect of Kegel exercises.
Pessaries
Urine leakage may be caused by a sagging uterus or a bulge or bend in the urethra. In these cases, a pessary may help. A pessary is a firm rubber ring that supports the bottom of your uterus. It can be inserted in the vagina by a physician and worn continuously.
Surgery
The most common cause of stress incontinence in women is lack of support at the bladder neck. Surgery can be used to treat this problem. It is usually considered when other treatments have been ineffective.
The goal of surgery is to wrap the urethra with a “sling” of fibrous tissue or loops of suture material. (The urethra is the drainage tube for the bladder.) The urethra is then tethered to the pelvis so it won’t sag or shift off center.
Surgery can be done through an incision above the pubic bone or in the vagina. In some cases, a needle-shaped instrument is used. After pain-killing medicine is injected, the instrument is inserted through the skin above the pubic bone or the front wall of the vagina.
Some specialized medical centers use robotic surgery. Instruments attached to metal rods are inserted into the pelvis through small incisions. The instruments on the rods are maneuvered by a surgeon. The surgeon uses a remote control while watching a magnified video screen.
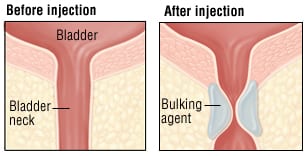
Occasionally, the bladder neck can be thickened by injecting a non-absorbable material. This can help some people to hold urine more easily.
Rarely, an electrical stimulator may be surgically implanted. This device periodically stimulates the nerve that controls bladder function and pelvic muscles. This may reduce symptoms in certain people who have urge incontinence or bladder overflow.
Other Strategies
If your urine leaks when you cough, seek treatment for your cough. If your cough results from smoking, talk to your doctor about ways to quit.
Pads or adult diapers can offer security. But they can also irritate the skin. They should not be the first or only treatment used for incontinence.
When To Call A Professional
If you experience urinary incontinence, tell your doctor. He or she can provide basic treatments for urinary incontinence. Some physicians specialize in evaluating and treating urinary incontinence. They are called urogynecologists or female urologists.
Prognosis
Most women who seek treatment for urinary incontinence find that their symptoms improve. Bladder retraining can lead to good results after only a few weeks. Kegel exercises improve urine control in many women who use them consistently.
Surgery for urinary incontinence can be very successful. But it can result in one or more complications. These include:
- Difficulty emptying the bladder
- Bladder spasms
- Bladder infection
- Injury to the bladder during surgery
- Return of incontinence
Additional Info
American Urological Association
1000 Corporate Blvd.
Linthicum, MD 21090
Phone: 410-689-3700
Toll-Free: 1-866-746-4282
Fax: 410-689-3800
http://www.urologyhealth.org/