Presence of rheumatic and musculoskeletal comorbidities were not associated with significant alterations in COVID-19 pneumonia-related clinical outcomes
1. There were no significant differences in symptom duration, length of hospital stay, and chest X-ray score between patients hospitalized for COVID-19 pneumonia with rheumatic and musculoskeletal diseases, compared to controls without these comorbidities.
2. Major risk factors for hospital admission and mortality included older age and pre-existing comorbidities (i.e. arterial hypertension and obesity).
Evidence Rating Level: 3 (Average)
Study Rundown: The novel coronavirus has caused significant morbidity and mortality globally, with Lombardy, Italy being among the most affected. This study assessed the trajectory of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in 117 patients with rheumatic and musculoskeletal diseases who were admitted to the Azienda Socio Sanitaria Territoriale (ASST) Spedali Civili of Brescia in Lombardy. The study also used a case-control design to compare patients with confirmed COVID-19 pneumonia with concurrent rheumatic and musculoskeletal diseases with age, sex and month of admission-matched in-patients with COVID-19 pneumonia without the same comorbidities. Study results showed that there were no significant differences in duration of COVID-19 symptoms, length of hospital stay, and X-ray Brixia score among patients with rheumatic and musculoskeletal diseases who were hospitalized for COVID-19 pneumonia (cases) compared to their counterparts without rheumatic or musculoskeletal comorbidities (controls). The study was limited by a small sample size and single-centre study design, potentially limiting generalizability of findings. Nonetheless, the study is the largest single-centre observational and case-control cohort of rheumatology patients with COVID-19 and shed light on next steps in this field.
Click here to read the study in The Lancet Rheumatology
Relevant Reading: GM-CSF blockade with mavrilimumab in severe COVID-19 pneumonia and systemic hyperinflammation: a single-centre, prospective cohort study
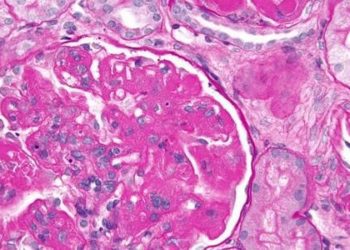
In-depth [prospective cohort and case-control study]: In this single-centre analysis in Lombardy, 117 (8%) patients with rheumatologic and musculoskeletal diseases were identified with confirmed (n=65) or suspected (n=52) COVID-19 between February 24 and May 1 2020. Using telephone and outpatient clinic-based surveys, data regarding the occurrence of SARS-CoV-2 infection symptoms, confirmed COVID-19 testing and demographic variables were collected. A case-control study with age, sex and month of hospital-matched controls not having rheumatologic or musculoskeletal disease was subsequently conducted, evaluating differences in disease course, radiologic findings, biomarkers of hyperinflammation and treatments received.
Overall, confirmed cases, relative to their suspected COVID-19 counterparts, were older (median age 57 years vs. 68 years, p=0.001], and had higher rates of arterial hypertension (27% vs. 51%, odds ratio [OR] 2.8, 95% confidence intervals [CI] 1.3 to 6.1, p=0.031) and obesity (2% vs. 17%, OR 11.0, 95% CI 1.3 to 83.4, p=0.0059). No differences were observed between confirmed and suspected cases with respect to use of glucocorticoids, conventional disease modifying antirheumatic drugs (DMARDs), and biologic agents. Among confirmed cases, 72% (47 of 65) were hospitalized; these patients were generally older than non-hospitalized confirmed cases (median age 70 years (IQR 60.5 to 76.0) vs. 54 years (IQR 47.0 to 73.8.), p=0.036].
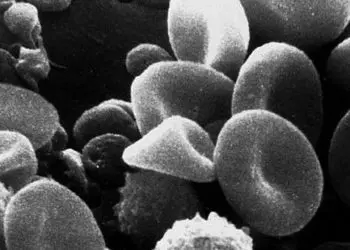
In the case-control study, 26 COVID-19 patients with rheumatic or musculoskeletal disease were matched to 62 COVID-19 infected controls without the same comorbidities, by age, sex, and month of hospital admission. Although no significant differences were noted for onset of COVID-19 symptoms, duration of hospital stay, and X-ray score, cases had more profound lymphopenia than controls (810 cells per mm3 vs. 560 cells per mm3, p=0.021). Rheumatoid arthritis (35%) comprised the majority of rheumatologic and musculoskeletal ailments among cases, followed by Still’s disease (12%), and polymyalgia rheumatica (12%). Intravenous or oral glucocorticoids were administered for 65% of cases, while tocilizumab was used for the remaining 25%. No significant differences in therapy were otherwise noted during hospital admission between cases and controls.
Image: PD
©2020 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.