Quantitative flow ratio-guided coronary intervention reduces the rate of major cardiac events compared to visual angiography
1. Quantitative flow ratio (QFR) allowed for better periprocedural assessment of stenoses, leading to a lower amount of unnecessary stenting procedures.
2. After 1 year, those who had underwent QFR-guided PCI had less adverse outcomes compared to angiography-guided.
Evidence Rating Level: 1 (Excellent)
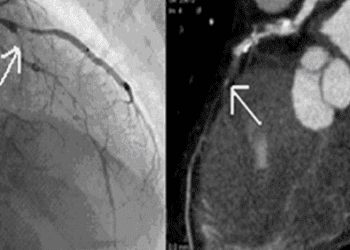
Study Rundown: During percutaneous coronary intervention (PCI), angiography remains the most common tool to visualize the arteries during the procedure. Another method is QFR-guided PCI, which estimates fractional flow reserve by using a pressure wire-based measurement to assess the extent of the stenosis in the coronary arteries. This study enrolled patients set to undergo a PCI procedure and all patients had a revascularization plan made by angiography. Patients were then randomized to undergo PCI guided by angiography or QFR. During the procedure, QFR allowed for a more accurate assessment of the stenoses visually identified for PCI. Notably, in around a fifth of patients in the PCI group, the original revascularization plan was changed because stenoses thought to be severe were found to be not hemodynamically obstructive by QFR. Overall, less stents were placed than originally planned in the QFR group, which correlated to fewer periprocedural myocardial infarctions. In some patients, this led to zero stents being placed. After the 1-year follow-up period, there were fewer events of the composite primary outcome in the group which had undergone QFR-guided PCI. Limitations of this study include only having a 1-year follow-up of clinical outcomes. Nevertheless, this study provides high-quality evidence for the implementation of QFR-guided PCI.
Click to read the study in the Lancet
Relevant Reading: Association between adherence to fractional flow reserve treatment thresholds and major adverse cardiac events in patients with coronary artery disease
In-Depth [randomized controlled trial]: This multicentre randomized control trial done across 26 hospitals in China included patients ages ≥18 years, with stable or unstable angina pectoris, or myocardial infarction at least 72 hours before screening. Exclusion criteria included moderate to severe kidney disease. Before randomization, each patient had a revascularization plan made by visual angiography. Patients were randomized 1:1 to receive either QFR-guided PCI or angiography-guided PCI. The primary outcome was a composite of major adverse cardiac events, all-cause mortality, myocardial infarction, and revascularization in the following year. A total of 3825 patients participated in the study with a mean age of 62.7 years and 29.4% women. Patients were masked to their group for the duration of the 1-year follow-up.
During the procedure, QFR changed the revascularization plans of 23.3% of patients due to the added information. In 19.6% of patients, a stent was deferred in stenoses that were found to be not hemodynamically obstructive. In 4.4% of patients, QFR led to the stenting of stenoses that were found to be more hemodynamically obstructive than originally identified by angiography alone. The primary outcome occurred in 5.8% of the QFR group and 8.8% of the angiographic group. A hazard ratio of 0.65 (95% CI 0.51 to 0.83, p=0.0004) was calculated between QFR versus angiography.
Image: PD
©2021 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.