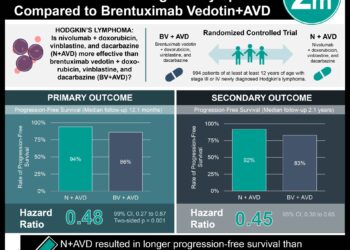
Rituximab after autologous stem cell transplantation in mantle cell lymphoma patients prolongs survival
1. Patients with mantle cell lymphoma treated with autologous stem cell transplantation experienced greater overall, event-free, and progression-free survival when treated with rituximab maintenance therapy compared to patients not receiving maintenance therapy.
2. Serious infection after transplantation was observed in equal numbers of patients in both the rituximab maintenance therapy and observation groups.
Evidence Rating: 1 (Excellent)
Study Rundown: Mantle cell lymphoma is a type of non-Hodgkin’s lymphoma in which relapse is common after treatment. Recent studies suggest residual tumor cells remaining after treatment may be responsible for relapses, indicating maintenance therapy may prove beneficial in reducing relapse risk. In this study, the monoclonal antibody rituximab was used in patients post autologous stem-cell transplant. This phase 3 clinical trial included non-senior adult patients with mantle cell lymphoma. After transplantation, patients were randomized to receive rituximab every 2 months for 3 years or undergo observation and followed to assess for event-free survival. Event-free survival in the rituximab group was greater than in the observation group at 4 years post randomization. Secondary endpoints including rate of progression-free survival and overall survival were also greater in the rituximab group than the observation group at 4 years. This study indicates suggests treatment with rituximab maintenance therapy after autologous stem cell transplantation prolongs survival in patients with mantle cell lymphoma.
Click to read the study, published today in NEJM
Relevant Reading: Landscape of somatic mutations and clonal evolution in mantle cell lymphoma
In-Depth [randomized controlled trial]: This phase 3 randomized clinical trial enrolled patients from 2008 to 2012. Adult, non-senior patients with untreated mantle cell lymphoma eligible to undergo autologous stem cell transplantation with multi-site disease were included in this study. All patients received induction chemotherapy, had autologous stem cells harvested, received a conditioning chemotherapy regimen, and underwent autologous stem cell transplantation. Patients were randomized into rituximab maintenance therapy (n = 120) and observation (n = 120) groups. Those in the rituximab group received a standard dose every 2 months for 3 years after transplantation. Patients were followed for a median period of 54.4 months, and outcomes assessed were event-free survival, progression-free survival, and overall survival. At 4 years, the rate of event-free survival was greater in the rituximab group (79%; 95%CI 70% to 86%) compared to the observation group (64%; 95%CI 51% to 70%; p = 0.001). Progression-free survival was greater in the rituximab group (83%; 95%CI 73% to 88%) versus the observation group (64%; 95%CI 55% to 73%; p < 0.001). Additionally, rate of overall survival at 4 years was greater in the rituximab group (89%; 95%CI 81% to 94%) versus the observation group (80%; 95%CI 72% to 88%; p = 0.04). The main toxic effects seen in the rituximab group was neutropenia. A second cancer was the cause of death in 3 rituximab treated patients and 1 observation patient, while 13 and 37 patients died in the rituximab and observation groups, respectively. Serious infection was observed in 4 patients in both groups.
Image: PD
©2017 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.