Social cohesion may reduce heart attack risk
1. Higher perceived neighborhood social cohesion was associated with lower risk of myocardial infarction after sociodemographic factors were considered.
2. A plateau effect was observed whereby social cohesion passed a certain level resulted in no additional risk benefits.
Evidence Rating Level: 3 (Average)
Study Rundown: Many individual and communal factors can have an impact on cardiovascular disease. This study sought to characterize the effect of neighborhood social cohesion on myocardial infarction (MI) using the National Institute on Aging’s Health and Retirement Study (HRS). Participants filled out a questionnaire describing their perceptions on togetherness, trust, and friendliness within their community. When sociodemographic factors were taken into consideration, the study found 22% lower odds of MI with each standard deviation increase in perceived social cohesion. The study also showed a decreased risk of MI when psychosocial, biological, and behavioral factors were individually added to the model. However, when all covariates were added to the model, the odds ratio (OR) only trended toward significance. In addition, when social cohesion was broken into quartiles, only comparing the highest and lowest groups showed significant differences in risk for some models. The authors point out that after a certain level of perceived social cohesion, the mean OR decreased very little with increasing perceived social cohesion.
While the results are the first to correlate myocardial infarction and an individual’s perception of their community, there are many limitations making the results difficult to interpret. When negative psychosocial factors were added to the model as a whole, the difference in MI risk was no longer significant. This may imply that overall satisfaction with one’s environment has an effect on MI rather than real differences in the social fabric. Further, the confidence intervals of many of the regression models were only slightly below 1. Additionally, the fact that only the groups with the lowest and highest perceived social cohesion scores showed a difference in OR brings into question whether the effect is large enough to strongly support the study’s conclusions. In line with this, because of the under-diagnosis of mood disorders in many communities, it is unclear whether this study can exclude the covariate of a generally negative outlook, which may be a better predictor of MI risk and would reframe the small effect size of this study as an indirect measure of a more salient feature. Finally, the study was only able to follow up patients within communities in the United States, and it is unclear how generalizable these results and conclusions are to communities across the world.
Click to read the study, published today in the BMJ
Relevant Reading: Neighborhood social interactions and risk of acute myocardial infarction
In-Depth [observational study]: This study covers 4 years of bi-annual follow-up data from HRS participants to evaluate the association of MI and perceived social cohesion. 7168 (age 51 to 105, mean = 70) respondents from the HRS study were selected for face-to-face interviews and were given a self-report psychological questionnaire that measured perceived social cohesion. 5276 (73.6% of total) participants with no history of myocardial infarction, of Caucasian, Black, or Hispanic populations, and returned the psychological questionnaire and were followed-up in the resultant analysis. 8 multiple regression models were used with various covariates considered in each. The models’ covariates were as follows; 1) age and gender, 2) age, gender, race/ethnicity, marital status, educational degree, and total wealth (“core” model, 3) core model + health behaviors (i.e. smoking, etc), 4) core model + biological factors, 5) core model + negative psychosocial factors, 6) core model + positive psychosocial factors, 7) core model + social engagement levels, and 8) all covariates. The core model showed an OR of 0.78 (CI95%, 0.63-0.94) for every increase in the SD of perceived social cohesion. All other models had significant ORs except model 5 (negative psychosocial factors) and model 8 (all covariates). When broken into quartiles, only the highest and lowest groups were significantly different in models 1 (age/gender), 2 (core), and 3 (health behaviors), while none of the other models had significantly different quartiles.
More from this author: Welfare Policies Increase Physician Workload in UK; Decreased facial expression variability linked with serious cardiac disease; HIV infection may protect against multiple sclerosis
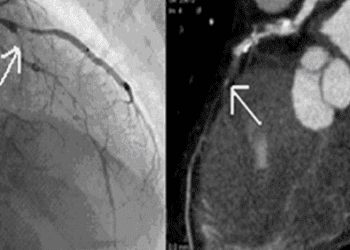
Image: PD
©2012-2014 2minutemedicine.com. All rights reserved. No works may be reproduced without expressed written consent from 2minutemedicine.com. Disclaimer: We present factual information directly from peer reviewed medical journals. No post should be construed as medical advice and is not intended as such by the authors, editors, staff or by 2minutemedicine.com. PLEASE SEE A HEALTHCARE PROVIDER IN YOUR AREA IF YOU SEEK MEDICAL ADVICE OF ANY SORT.