Tolebrutinib not superior to teriflunomide in reducing relapsing multiple sclerosis relapse rates
1. In concurrent randomized controlled trials (GEMINI 1 and GEMINI 2) of patients with relapsing multiple sclerosis (RMS), tolebrutinib did not significantly reduce relapse rates compared to teriflunomide.
2. The incidence of adverse events was similar between the tolebrutinib and teriflunomide groups, with no significant differences.
Evidence Rating Level: 1 (Excellent)
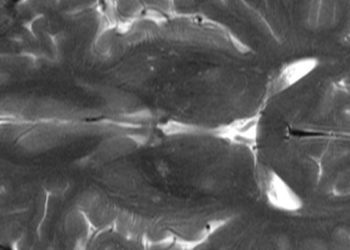
Study Rundown: Multiple sclerosis is characterized by the formation of white matter lesions leading to neurological deficits. Disease-modifying therapies aim to reduce clinical relapses, the formation of focal lesions on MRI, and the progression of disability. Tolebrutinib, an inhibitor of Bruton’s tyrosine kinase (BTK) involved in myeloid cell signaling, has been proposed as a potential treatment for relapse control in multiple sclerosis. Two concurrent randomized controlled trials (GEMINI 1 and GEMINI 2) evaluated the efficacy and safety of tolebrutinib compared to teriflunomide, an established disease-modifying therapy, in preventing relapses and disability progression. There was no significant difference in the annualized relapse rate between the two groups. Although not statistically significant, participants receiving Tolebrutinib showed a lower incidence of confirmed disability worsening sustained for at least six months and a higher incidence of sustained disability improvement compared to the teriflunomide group. However, tolebrutinib was associated with a higher adjusted mean number of new gadolinium-enhancing lesions on T1-weighted MRI. The overall incidence of adverse events was comparable between groups. It is important to note that this study only compared tolebrutinib to teriflunomide and did not include other MS therapies. Overall, tolebrutinib did not demonstrate superior efficacy in reducing relapse rates or inflammatory activity.
Click here to read the study in NEJM
Relevant Reading: Tolebrutinib in Nonrelapsing Secondary Progressive Multiple Sclerosis
In-Depth [randomized controlled trial]: Two randomized controlled trials, GEMINI 1 and GEMINI 2, evaluated the efficacy and safety of tolebrutinib in comparison to Teriflunomide for treating relapsing multiple sclerosis. Participants were aged 18 to 55, met the 2017 McDonald criteria for relapsing MS, had an Expanded Disability Status Scale (EDSS) score of 5.5 or lower, and had either one relapse in the past year, two in the past two years, or a gadolinium-enhancing brain lesion on MRI within the previous year. Patients with primary progressive or non-relapsing MS were excluded. The adjusted annualized relapse rate was 0.13 with tolebrutinib and 0.12 with Teriflunomide (rate ratio, 1.06; 95% Confidence Interval [CI], 0.75–1.32; p = 0.98), indicating no significant difference. However, 8.3% of participants on tolebrutinib experienced six-month confirmed disability worsening versus 11.3% in the teriflunomide group (hazard ratio, 0.71; 95% CI, 0.53–0.95), while 12.6% had six-month sustained disability improvement compared to 10.4% with teriflunomide (hazard ratio, 1.22; 95% CI, 0.94–1.60). MRI results favored teriflunomide, as tolebrutinib was associated with more gadolinium-enhancing lesions on T1-weighted imaging: GEMINI 1 (adjusted rate ratio, 1.86; 95% CI, 1.36–2.55) and GEMINI 2 (adjusted rate ratio, 2.12; 95% CI, 1.50–2.99). Similarly, T2-weighted imaging showed a modest increase in new or enlarging lesions with tolebrutinib in GEMINI 1 (adjusted rate ratio, 1.08; 95% CI, 0.88–1.34) and GEMINI 2 (adjusted rate ratio, 1.17; 95% CI, 0.91–1.50). Adverse events were similar between groups, reported in 84.9% of participants on tolebrutinib and 86.3% on teriflunomide. Elevations in alanine aminotransferase greater than three times the upper limit of normal were observed in 5.6% and 6.3% of participants, respectively. In summary, tolebrutinib did not reduce relapse rates compared to Teriflunomide but showed some potential for disability improvement, though with increased MRI activity.
Image: PD
©2025 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.