2 Minute Medicine Rewind August 18, 2025
1. In this cohort of individuals with type 2 diabetes (T2D), use of Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) is associated with a slightly increased risk of developing diabetic retinopathy (DR); however, it is also associated with fewer severe vision-threatening complications.
Evidence Rating Level: 2 (Good)
Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) are antihyperglycemic medications used in individuals with type 2 diabetes (T2D) for sugar control and weight loss. Currently, they are recommended as one of the main treatments for T2D, especially in those with cardiovascular disease. However, some previous studies have found associations between GLP-1 RAs and developing diabetic neuropathy (DR) and increased risk of nonarteritic anterior ischemic optic neuropathy (NAION), while other studies have not found this evidence. To better add on to previous research, this retrospective cohort study was conducted on individuals with T2D and a hemoglobin A1C of 6.5% or higher. The treatment group included individuals who received a prescription for a GLP-1 RA, while the control group included those who did not. After meeting the inclusion criteria, 185,066 (mean [SD] age, 59.0 [12.5] years) individuals were prescribed a GLP-1 RA. During follow-up, both groups had 2.7% of individuals (5,037 in the GLP-1 RA group and 4938 in the control group) develop incident DR (n=185,066 per group; HR, 1.07; 95% CI, 1.03-1.11; P=.001). The treatment group had an increased risk of NAION (96 [0.1%] vs 79 [<0.1%] events; HR, 1.26 [95% CI, 0.94-1.70]; P=.12) and ischemic optic nerve conditions (243 [0.1%] vs 230 [0.1%] events; HR, 1.10 [95% CI, 0.92-1.32]; P=.31), however, this was not statistically significant. Treatment with GLP-1 RA did not significantly affect the risk of developing proliferative diabetic retinopathy (PDR) (1121 of 32,695 [3.4%] vs 1039 of 32,695 [3.2%] events; HR, 1.06 [95% CI, 0.97-1.15]; P=.18) or new cases of diabetic macular edema (DME) (7390 [22.6%] vs 7425 [22.7%] events; HR, 0.98 [95% CI, 0.95-1.01]; P=.25).
1. In this randomized controlled trial, all three ultrasound-guided treatments for mild to moderate carpal tunnel syndrome (CTS) improved pain and function, with pulsed radiofrequency and steroid injections having the greatest effect.
Evidence Rating Level: 1 (Excellent)
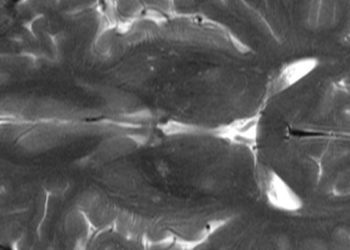
Carpal tunnel syndrome (CTS) is a commonly occurring compression neuropathy affecting the median wrist nerve, presenting with increased endoneurial pressure, reduced neuronal microcirculation, neural ischemia, edema, and fibrosis. While some other non-surgical options have been explored, including splints and physical therapy, they have proven to provide only mild relief. Some newer modern treatment options have been investigated, the mechanisms of which are only moderately understood. The goal of this study was to compare the efficacy of pulsed radiofrequency (PRF) against platelet-rich plasma (PRP) injections in the treatment of mild to moderate idiopathic cases of CTS. The double blind randomized controlled trial was conducted on patients who had experienced mild CTS for more than 3 months who did not respond to traditional treatment. In all groups, a significant reduction was seen in the Visual Analog Scale (VAS), with inter-group differences observed at one week, two months and four months (all p<0.001). PRF resulted in greater improvements than both PRP and control for pain and function scores on the Boston Carpal Tunnel Questionnaire, while PRP and control did not significantly differ. For median nerve cross-sectional area, PRP was better than control (p=0.002), and PRF was superior to PRP (p<0.001). Overall, the PRF group showed the greatest improvement over four months, with minimal differences seen between control and PRP, likely due to the short-term effects of steroids. Overall, while all treatments, combining ultrasound-guided hydrodissection with another treatment, showed improvements in mild CTS cases, PRF and steroid injection provided the most relief.
Work Impairment and Financial Outcomes Among Adults With vs Without Long COVID
1. In this cohort of adults with SARS-CoV-2 infection, participants with current long COVID (LC) experienced increased financial stress, work impairment, and more days of missed work than those without LC.
2. Vaccination was associated with better work productivity and lower financial strain, regardless of LC status.
Evidence Rating Level: 1 (Excellent)
Over 777 million cases of COVID-19 have been reported globally, and approximately 13% of infected individuals develop long COVID (LC), where symptoms persist for at least three months. Common symptoms of LC include fatigue, dyspnea, and cognitive issues, which may significantly impact quality of life. Much of the previous research has focused on health outcomes, and there is limited knowledge about how LC affects work productivity and financial well-being. To fill these gaps, the INSPIRE study aims to assess return to work, work productivity, and financial toxicity among people with LC, resolved LC, and no LC in the United States. Eligible participants completed a survey responding with their COVID-19 symptoms and history to assess if the participants had LC. The study measured work impairment using the WPAI questionnaire, which assessed missed work hours, impaired work hours, overall work impairment, and non-work activity impairment. To evaluate the financial impact, the Functional Assessment of Chronic Illness Therapy Comprehensive Score for Financial Toxicity (FACIT-COST) was used, with lower scores indicating greater financial strain. A total of 3663 eligible individuals (mean [SD] age, 40.2 [14.2] years) were included in the study. Among them, 994 (27.1%) had current LC, 65 (1.8%) had resolved LC, and 2604 (71.1%) had never had LC. Participants with current LC missed an average of 6.2% (SD 19.4%) of their scheduled work hours, significantly more than those with resolved LC (2.7%, SD 9.3%) or no LC (2.1%, SD 10.7%) and had over twice the odds of missing work due to health (aOR, 2.62; 95% CI, 1.93-3.57). When analyzing financial strain, participants with current LC were significantly more likely to experience moderate to high financial toxicity compared to those without LC (aOR, 5.20; 95% CI, 3.92-6.89) and those with resolved LC (aOR, 3.16; 95% CI, 1.19-8.41). Vaccinated participants experienced less overall work impairment (aOR, 0.71; 95% CI, 0.50-0.92), less impairment while working (aOR, 0.66; 95% CI, 0.50-0.87), less impairment in nonwork activities (aOR, 0.74; 95% CI, 0.57-0.96) and lower financial toxicity (mean difference 1.07; 95% CI, 0.19-1.95) compared to unvaccinated participants. In summary, this long-term cohort study found that individuals with current long-term COVID experienced significantly more work impairment, missed work, and financial toxicity compared to those without long COVID.
1. In this randomized clinical trial of children with upper limb burn injuries, active video games (AVGs) significantly reduced pain and improved wrist joint mobility.
Evidence Rating Level: 1 (Excellent)
Burn injuries are a major cause of death and disability in children, often resulting in long-term muscle loss, joint dysfunction, and limited mobility, particularly in the hands, elbows, and shoulders. Up to 42% of severe burn patients experience joint issues by discharge, significantly impacting daily activities and quality of life. A good recovery requires a multidisciplinary approach, combining acute care, rehabilitation, pain management, and psychological support to ensure proper healing and avoid complications. Interactive tools such as virtual reality (VR) and active video games (AVGs) have increased in popularity in pediatric rehabilitation due to their engaging, multisensory nature. However, evidence on their effectiveness, specifically for pain relief, range of motion (ROM), and motor function in pediatric burns, has remained limited. To address this gap, the study aims to evaluate the impact of AVGs on these aforementioned outcomes in children with upper limb burns, especially in resource-limited settings. To achieve this, a randomized clinical trial was conducted at the Imam Reza Hospital in Iran, comparing the effectiveness of AVGs to conventional physiotherapy. Three main outcomes were measured, including pain intensity using the Wong-Baker FACES scale, joint ROM at the wrist, elbow, and shoulder using a goniometer, and motor function using the Activities Scale for Kids (ASK) were assessed before and after intervention. A total of 70 children were equally randomized to the intervention group (n=35) and the control group (n=35). During the pre-intervention phase, there was no significant difference in pain scores between the groups (p>0.05). However, by the second week, the intervention group had a statistically significantly lower mean pain score (3.17 ± 0.38) compared to the control group (4.26 ± 0.51) (P<0.05; 95% CI: -1.3, -0.87). The intervention group experienced a significantly greater improvement in wrist joint ROM compared to the control group (p<0.001; 95% CI: 2.61-10.62). However, there were no significant differences between the groups for shoulder (p=0.490, 95% CI: -39.91-26.86) or elbow ROM (p=0.060; 95% CI: -1.70 to 19.14). Between the groups, there were no significant differences for motor function (p=0.058, 95% CI: -0.16-9.68). In summary, this randomized clinical trial provided new evidence supporting the use of AVGs for children with upper limb burn injuries.
1. In this cohort of women living with HIV (WLWH) in Rwanda, there was an increased risk of delivering a low birth weight (LBW) baby compared to women unaffected by HIV.
2. Among the WLWH, starting antiretroviral therapy (ART) before pregnancy was associated with a decreased risk of LBW.
Evidence Rating Level: 2 (Good)
In 2010, the World Health Organization (WHO) recommended triple antiretroviral therapy (ART) for pregnant women living with HIV during pregnancy and breastfeeding. By 2013, these options expanded to lifelong ART regardless of CD4 counts. By 2015, most women receiving ART for prevention of mother-to-child transmission (PMTCT) were on lifelong therapy, resulting in decreased HIV transmission to infants. However, millions of HIV-uninfected infants are now exposed to ART during pregnancy and breastfeeding, with limited knowledge on the long-term effects. With the near-universal ART coverage and growing population of children who are HIV-exposed and uninfected (CHEU), updated evidence on pregnancy outcomes such as low birth weight (LBW) is crucial. This retrospective cohort study addressed the gap by examining adverse birth outcomes among women living with HIV and HIV-uninfected women in Rwanda. The main endpoint was low birth weight, defined as less than 2,500 g, while the secondary endpoints included stillbirth and preterm birth. Of 10,191 eligible women with HIV, 12.7% (n=1,293) were women living with HIV (WLWH). Compared to women without HIV, WLWH had higher rates of LBW babies (2.9% vs 6.5%, p<0.001) and stillbirths (0.4% vs 0.6%, p=0.02), whereas the prevalence of preterm birth was similar (0.5% vs 0.7%, p=0.9). Even after accounting for other factors such as marital status, maternal weight at delivery, and gravida status, HIV positive status was associated with LBW (aOR 1.61; 95% CI, 1.08, 2.39; p<0.05). In WLWH who started ART before pregnancy, there was a 50% decreased odds of delivering a LBW baby compared to WLWH who started ART during pregnancy (OR 0.9; 95% CI 0.52, 1.56). Overall, these results indicate the importance of receiving early HIV diagnosis and treatment, particularly in the prenatal phase.
Image: PD
©2025 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.