2 Minute Medicine Rewind August 4, 2025
Initiation of Pregabalin vs Gabapentin and Development of Heart Failure
1. In patients aged 65 to 89 years of age with non-cancer chronic pain, use of pregabalin was associated with an increased risk of developing heart failure (HF) compared with gabapentin.
Evidence Rating Level: 2 (Good)
Pregabalin and gabapentin are commonly prescribed medications for the management of chronic pain. While both medications may be associated with cardiovascular adverse effects based on limited reports, existing studies have limited their analyses to neurological indications or have not focused on older adults. This retrospective cohort study therefore sought to investigate the incidence of HF in older adults using pregabalin compared with gabapentin. 246,237 patients (median age[IQR], 73[69-78] years; 66.8% female) aged 65 to 89 years of age receiving pregabalin or gabapentin for chronic pain without a history of HF from the United States were included in this study. The primary endpoint was hospitalization or ED visit with a diagnosis of HF, with secondary endpoints including a diagnosis of HF in the outpatient setting. The incidence of HF with pregabalin was 18.2 (95% CI, 15.3-21.6) per 1000 person-years compared to 12.5 (95% CI, 11.9-13.2) per 1000 person-years for gabapentin, with a corresponding adjusted hazard ratio (AHR) for pregabalin vs gabapentin of 1.48 (95% CI, 1.19-1.77). Additionally, there was a higher incidence of outpatient diagnosis of HF in patients receiving pregabalin compared to gabapentin (AHR, 1.27 [95% CI, 1.02-1.58]). Overall, this study found that among older patients with non-cancer chronic pain, management with pregabalin was associated with higher risk of HF compared with gabapentin.
Initiation of Antiseizure Medications in Patients With Brain Abscess
1. In patients with a brain abscess, use of antiseizure medications (ASM) was not associated with a statistical difference in the risk of epilepsy at 90, 135 and 180 days after initiation of ASMs.
Evidence Rating Level: 2 (Good)
Epilepsy is a common complication of brain abscesses, yet the literature surrounding the appropriate management of epilepsy in the setting of a brain abscess is limited. Indeed, there have been limited efforts to investigate the effectiveness of ASMs in preventing epilepsy in brain abscess survivors. This retrospective cohort study therefore sought to assess the efficacy of ASMs in reducing epilepsy risk in patients with brain abscesses. 572 adult patients (mean[SD] age, 61.5[16.6] years; 61.6% male) from the United States with a documented acute care visit for brain abscess without prior history of epilepsy were included in the study. These patients were separated into a treatment group defined by having initiation of ASM within 45 days after the index date (n = 478) and no ASMs (n = 94). The primary outcome of the study was a diagnosis of epilepsy or seizures at 15 or greater days after the index date. There was no statistical difference in the incidence of epilepsy at 15 days or greater following the index date, with the marginal risk difference (RD) at 90 days being –0.02% [95% CI, −4.9% to 4.8%], at 135 days being 1.9% [95% CI, −5.0% to 8.5%] and at 180 days being 3.5% [95% CI, –4.4% to 10.8%]. Overall, this study found that the use of ASMs was not associated with a reduced risk of epilepsy.
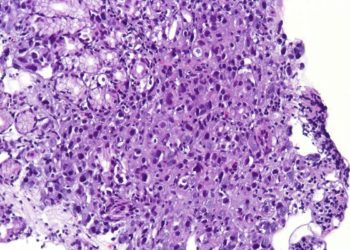
Efficacy and Safety of Ustekinumab and Vedolizumab for Crohn’s Disease of the Pouch
1. In patients with Crohn’s disease (CD) of the pouch following ileal-pouch anal anastomosis (IPAA) for medically-refractory ulcerative colitis (UC), the clinical response at 3 and 6 months was significantly greater for ustekinumab (UST) compared to vedolizumab (VDZ).
Evidence Rating Level: 2 (Good)
A significant number of patients living with UC will eventually require IPAA, from which as high as 17% of patients will develop CD of the pouch. Historically, management of CD of the pouch has been limited to antitumour necrosis factor alpha therapies such as infliximab. However, the efficacy and safety of newer inflammatory bowel disease (IBD) therapies in the management of CD of the pouch, including UST and VDZ, have not been investigated. This retrospective cohort study therefore sought to investigate the clinical and endoscopic outcomes associated with the management of CD of the pouch with UST and VDZ. 104 adult patients who received either UST (N = 77; mean[SD] age, 44.4[14.6] years) or VDZ (N = 57; mean[SD] age, 46.9[15.3] years) or both for CD of the pouch following IPAA for UC from several centres across the United States were included in this study. The primary outcome was clinical response after 3 and 6 months, with secondary outcomes including clinical remission and endoscopic outcomes. At 3 months, the clinical response was greater in UST at 62% (48/77) compared with 53% (30/57) for VDZ (P = .34). Similarly, at 6 months the clinical response was 56% (43/77) for UST and 46% (26/57) for VDZ (P = .32). Endoscopic response was also greater with UST (41% [25/61]) after a median follow-up of 1 year compared with VDZ (27% [12/44]). Under multivariate analysis, UST had a significantly greater 3-month clinical response (odds ratio [OR] 2.73, 95% confidence interval [CI]: 1.13-6.56, P = .025) and 6-month clinical response (OR 2.53, 95% CI: 1.01-6.29, P = .046) compared to VDZ. Overall, this study found that among patients with CD of the pouch following IPAA for UC, the clinical response with UST was significantly greater compared with VDZ at 3 and 6 months.
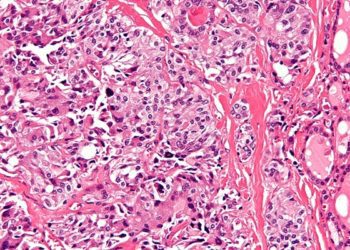
1. In patients with metastatic pancreatic cancer, neither modified fluorouracil, leucovorin, irinotecan and oxaliplatin (mFOLFIRINOX) or S-1, irinotecan and oxaliplatin (S-IROX) demonstrated improved clinical benefits compared with nab-paclitaxel and gemcitabine.
Evidence Rating Level: 1 (Excellent)
The vast majority of patients with pancreatic cancer have metastatic disease at diagnosis, with a poor prognosis. The standard of care for metastatic pancreatic cancer includes systemic chemotherapy regimens such as mFOLFIRINOX and nab-paclitaxel plus gemcitabine. As there have been no direct comparisons in the literature between these regimens, this randomized phase II/III trial sought to compare mFOLFIRINOX, S-IROX and nab-paclitaxel plus gemcitabine for the management of metastatic or recurrent pancreatic cancer. Between April 2019 and March 2023, 527 patients with metastatic pancreatic cancer from Japan were enrolled and randomly assigned to receive either nab-paclitaxel and gemcitabine (N = 176; median[IQR] age, 65[57-70] years), mFOLFIRINOX (N = 175; median[IQR] age, 67[59-71] years) or S-IROX (N = 176, median[IQR] age, 65[57-70]). The primary endpoint of the phase II portion of the trial was objective response rate (ORR) in the S-IROX group, while the primary endpoint of the phase III portion was overall survival (OS) in all patients. The median OS was highest in the nab-paclitaxel group at 17.0 months (95% CI, 14.5 to 18.9) compared with 14.0 months (95% CI, 11.4 to 16.3) in the mFOLFIRINOX group (HR, 1.29 [95% CI, 0.98 to 1.70]) 13.6 months (95% CI, 12.3 to 16.3) in the S-IROX group (HR, 1.29 [95% CI, 0.98 to 1.70]). During the phase III portion, the ORRs were 35.4% (95% CI, 28.4 to 43.0) in the nab-paclitaxel plus gemcitabine group, 32.4% (95% CI, 25.4 to 39.9) in the mFOLFIRINOX group, and 42.4% (95% CI, 34.8 to 50.2) in the S-IROX group. Overall, this study found that mFOLFIRINOX and S-IROX did not demonstrate improved survival benefits compared with nab-paclitaxel and gemcitabine.
1. In septic patients with liver cirrhosis, the neutrophil-to-lymphocyte (NLR) ratio was positively correlated with all-cause mortality.
Evidence Rating Level: 1 (Good)
Sepsis-related mortality among patients with liver cirrhosis is much greater than in patients without liver cirrhosis. NLR has been previously shown to be a reliable predictor of mortality in other inflammation-related diseases such as malignant tumours, yet investigations into the role of NLR as a prognostic marker in septic patients with liver cirrhosis remain limited. This retrospective cohort study therefore sought to investigate the association of NLR with mortality risk in septic patients with liver cirrhosis. 1372 patients from the Beth Israel Deaconess Medical Center between 2008 and 2019 with sepsis and liver cirrhosis were included in the study. The primary outcome was all-cause mortality during hospitalization. NLR was significantly associated with all-cause mortality in both unadjusted (Odds Ratio (OR): 1.03, 95% CI: 1.02–1.04) and adjusted models (Model I: OR: 1.03, 95% CI: 1.01–1.04; Model II: OR: 1.02, 95% CI: 1.00–1.04). When compared with neutrophils alone or Sequential Organ Failure Assessment (SOFA) scores, NLR demonstrated a superior predictive value (area under the curve (AUC) = 0.752 versus 0.711 and 0.711 for neutrophils and SOFA scores). Overall, this study found that the NLR ratio was significantly correlated with all-cause mortality.
Image: PD
©2025 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.