2 Minute Medicine Rewind February 1 – February 8, 2015
In this section, we highlight the key high-impact studies, updates, and analyses published in medicine during the past week.
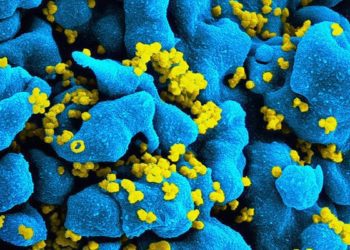
Tenofovir-Based Preexposure Prophylaxis for HIV Infection among African Women
Pre-exposure prophylaxis with tenofovir combined with or without emtricitabine has been shown to significantly reduce rates of HIV acquisition in populations including men who have sex with men, heterosexuals, and injection drug users when there are high rates of adherence. However, the effectiveness of prophylaxis with oral and intravaginal medications used by women in real life settings has not been thoroughly investigated. In this randomized control trial, 5,029 women in South Africa, Uganda, and Zimbabwe were randomized to receive daily treatment with oral tenofovir (TDF), oral tenofovir-emtricitabine (TDF-FTC), 1% tenofovir (TFV) vaginal gel, or a pill or gel placebo. Investigators found that in a modified intention-to-treat analysis, the hazard ratio for HIV-1 acquisition for intervention compared to placebo was 1.59 (95% CI 0.97-2.29, p=0.07), 1.04 (0.73-1.49, p=0.81), and 0.85 (0.61-1.21, p=0.37) for TDF, TDF-FTC, and TFV respectively. Researchers also found that by random sample, tenofovir was detected in the serum of 30%, 29%, and 25% of participants who received TDF, TDF-FTC, and TFV respectively. This study therefore showed that among women from several African countries there were low rates of adherence to pre-exposure prophylaxis regimens and that under these conditions there was no significantly observable reduction in the acquisition of HIV-1.
Underlying Reasons Associated With Hospital Readmission Following Surgery in the United States
The Centers for Medicare and Medicaid Services have begun to include rates of hospital readmission after surgical procedures as new measurements of care quality. However, the rates of and reasons for hospital readmission after different surgical operations have not been well characterized. From January 1, 2012 to December 31, 2012, the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) looked at re-admissions data for 498,875 operations (limited to bariatric procedures, colectomy or proctectomy, hysterectomy, total hip or knee arthroplasty, ventral hernia repair, lower extremity vascular bypass) across 346 US hospitals. Investigators found that there was a 5.7% unplanned readmission rate with these rates being highest for lower extremity vascular bypass (14.9%) and lowest for hysterectomy (3.8%). The most common reason for readmission was surgical site infection (SSI) which occurred in 19.5% of all readmissions. The second most common reason was obstruction or ileus which precipitated 10.3% of all readmissions. Interestingly, only 2.3% of patients were readmitted for a complication that they had experienced during their initial hospital stay, and only 3.3% of the patients readmitted with an SSI had an SSI during initial hospitalization. Investigators found that patient comorbidities, index surgical admission complications, non-home discharge (HR 1.40, 95% CI 1.35-1.46), teaching hospital status (1.14, 1.07-1.21), and higher surgical volume (1.15, 1.07-1.25) were all associated with a higher rate of readmission. This study helped characterize the complications that cause hospital readmission and has revealed that these complications are often new developments and due to post-discharge difficulties.
Rapid hemorrhage control is currently managed most frequently with the early administration of blood products in the unit ratio of 1:1:1 for plasma, platelets, and red blood cells (RBCs). While earlier studies showed that giving blood products was beneficial when compared with resuscitation with crystalloid solution, the effectiveness of this ratio compared to resuscitation with lower amounts of plasma and platelets has not been directly studied. It is thought that higher volumes of plasma containing products may induce greater deleterious inflammatory responses. In this randomized control trial, 680 patients who arrived at trauma centers and required massive transfusion were given either a 1:1:1 or a 1:1:2 blood product ratio. Investigators found that at 24 hours there was no significant difference in mortality between the groups (12.7% vs. 17.0% for the 1:1:1 and 1:1:2 groups respectively, difference of -4.2%, 95% CI -9.6-1.1%, p = 0.12). This held true at 1 month (22.4% vs. 26.1%, difference of -3.7%, -10.2 – 2.7%, p = 0.26). While the 1:1:1 group had significantly less death from exsanguination (9.2% vs. 14.6%, difference of -5.4%, -10.4- -0.5%, p = 0.03) and more hemostasis (86% vs. 78%, p = 0.006) in the first 24 hours, there was no significant difference between the two groups in incidence of acute respiratory distress syndrome, multiple organ failure, venous thromboembolism, sepsis, and transfusion-related complications. This study therefore showed that early administration of plasma, platelets, and RBCs in a 1:1:1 ratio was no different when compared to a 1:1:2 ratio with regards to mortality but did achieve greater rates of hemostasis and better prevented death from exsanguination at 24 hours.
Efficacy of a Device to Narrow the Coronary Sinus in Refractory Angina
An increasing number of patients with severe coronary artery disease are not candidates for revascularization and suffer from debilitating angina that persists despite maximal medical therapy. The company Neovasc has developed a balloon-expandable, stainless steel, hourglass-shaped device that fits in the coronary sinus and cause sinus narrowing with the goal of increasing upward sinus pressure and thus perfusion to ischemic myocardium. In this phase 2, randomized control trial, 104 patients with Canadian Cardiovascular Society (CCS) class III or IV angina received either this device or a sham procedure. At 6 months, 35% of the patients in the treatment control had an improvement in at least two CCS angina classes in comparison to 15% of the control group (p = 0.02). Similarly, 71% of patients in the treatment group had improvement in one CCS angina class in comparison to 42% in the control group (p = 0.003). There was also an observed improvement in the quality of life in the treatment group as assessed by the Seattle Angina Questionnaire (17.6 point improvement vs. 7.6 point, p = 0.03). However, there was no significant difference observed by dobutamine echocardiography or exercise stress test. This trial therefore shows that patients with unrevascularizable coronary disease and ongoing angina have significant improvement in their angina symptoms when given a novel coronary sinus narrowing device.
Effects of RAS inhibitors on diabetic retinopathy: a systematic review and meta-analysis
Several studies have looked at the potential beneficial effect of renin-angiotensin system (RAS) inhibitors on diabetic retinopathy. However, the results have been conflicting. In this systematic review and meta-analysis, researchers included data from 21 randomized control trials involving 13,823 patients. They found that RAS inhibitors resulted in a statistically significant reduced risk of diabetic retinopathy progression (RR 0.87, 95% CI 0.80-0.95, p = 0.002) and also increased the possibility of disease regression (RR 1.39, 95% CI 1.19-1.61, p = 0.00002). This was seen mainly in normotensive patients on RAS inhibitors, and there was no statistically significant difference in diabetic retinopathy progression or regression rates in hypertensive patients on RAS inhibitors. Overall it was shown that for preventing diabetic retinopathy progression, the most effective agents were ACE inhibitors followed by ARBs, beta blockers, calcium channel blockers and then placebo. With regards to diabetic retinopathy regression, the the most effective agents were ACE inhibitors followed by ARBs, placebo, and then calcium channel blockers. This meta-analysis therefore demonstrates that in patients with diabetes, RAS inhibitors (ACE inhibitors more than ARBs) are able to prevent the progression and increase rates of regression of diabetic retinopathy.
Image: PD
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.