2 Minute Medicine Rewind July 21, 2025
1. In this prospective cohort of pregnant individuals, the majority of the population was at an increased risk of preeclampsia based on criteria from the US Preventive Services Task Force (USPSTF)
Evidence Rating Level: 1 (Excellent)
Preeclampsia is a common cause of pregnancy-related morbidity and mortality, affecting approximately 8% of all pregnancies. The rate of hypertensive disorders in pregnancy has increased along with the rate of maternal mortality in the United States. As a result of these harrowing numbers, the US Preventive Services Task Force (USPSTF) recommends preeclampsia risk assessments. Based on a set of criteria, if a pregnant individual has at least one high-risk factor or two moderate-risk factors, they should initiate low-dose aspirin prophylaxis between 12 and 28 weeks of gestation. This cohort study was undertaken to determine the number of patients who fall into low, moderate, and high-risk categories based on the established criteria. The total study population was 5684 participants (median [IQR] age, 30.9 [26.4-33.6] years), with 5046 (88.8%) participants at an increased risk of developing preeclampsia (3996 [70.3%] at moderate risk and 1050 [18.5%] at high risk). Among the participants, the rate of preeclampsia overall was 12.1%. In participants with two or more moderate risk factors, nulliparity was associated with an increased risk of preeclampsia (RR, 1.48; 95% CI, 1.35-1.62; P<.001), while advanced maternal age (AMA) was associated with a decreased risk (RR, 0.79; 95% CI, 0.65-0.96; P=.02). Aspirin prophylaxis (AP) was recommended to almost half of the participants (46.7%) with 1 or more risk factors. Of those in the high-risk group, 82.0% (856 of 1044 participants) received an AP recommendation, whereas in the moderate risk group, only 37.4% (1486 of 3974 participants) received an AP recommendation. In this prospective observational cohort study, 89% of participants had at least 1 USPSTF preeclampsia risk factor. These results suggest that moderate risk factors alone offer little value in predicting preeclampsia, leading to overly broad AP use.
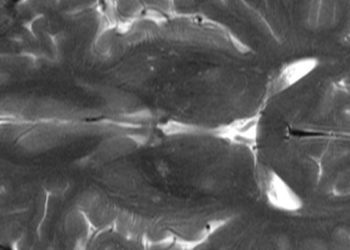
Long-Term Risk of Recurrent Cervical Artery Dissection and Stroke After Pregnancy
1. Among women with a history of cervical artery dissection (CeAD), pregnancy was not associated with an increased risk of recurrent CeAD, ischemic stroke, intracerebral hemorrhage, or death.
Evidence Rating Level: 2 (Good)
In women of childbearing age, the most common cause of stroke is cervical artery dissection (CeAD). Pregnancy and the postpartum period may increase the risk due to changes in hormones and the cardiovascular system. Although CeAD is rare, if it occurs, it is a significant complication during this time. There has been limited research on the risk of stroke in women with a history of CeAD who later became pregnant. To address this gap, an international cohort study was conducted to compare outcomes between women with prior CeAD who became pregnant and those who did not. In this study, pregnancy following CeAD, the exposure variable, was defined as the time from the onset of pregnancy to the end of the postpartum period, extending up to six weeks after delivery. To achieve the goal of the study, the primary outcomes were recurrent CeAD, ischemic stroke or intracerebral hemorrhage, and all-cause mortality. A total of 1013 patients (median [IQR] age, 42 [35-48]) were included in the study, of which 114 (11.3%) had 1 or more pregnancies after initial CeAD (pregnancy group), while 899 (88.7%) did not have further pregnancies (comparison group). The composite primary outcome was reported in 7.4% of all participants (75 of 1,013), with a slightly higher incidence in the pregnancy group (10 of 114; 8.8%) compared to the nonpregnancy group (65 of 899; 7.2%) (unadjusted HR 1.08, 95% CI, 0.56-2.08; age-adjusted hazard ratio, 0.77; 95% CI, 0.38-1.56). Among the pregnancy group, 7 patients had recurrent CeADs, 2 had ischemic strokes, and 1 had an intracerebral hemorrhage; of these events, 5 occurred postpartum. In comparison, in the nonpregnancy group, 32 patients had recurrent CeADs, 26 had ischemic strokes, 4 had an intracerebral hemorrhage, and 5 died. Overall, this cohort study found no evidence that pregnancy after CeAD was associated with an increased risk of CeAD recurrence, stroke, or mortality.
1. In this cohort study, dementia diagnosis was associated with increased levels of unmet social support needs, with notable differences based on race/ethnicity groups and sex.
Evidence Rating Level: 1 (Excellent)
Dementia and cognitive impairment involve a decline in cognition and memory, gradually resulting in functional impairments including disorientation, communication difficulties, and impaired judgement. These impairments place a significant burden on the affected individuals, families, and the healthcare system. Past research has focused on care after hospital discharge, and there is limited quantitative evidence on support continuity following a dementia diagnosis, especially during transitions to community care. This study used data from the Health and Retirement Survey (HRS) with a matched ambidirectional cohort design to examine how unmet social support needs evolve before and after diagnosis. The exposure group consisted of individuals with a dementia diagnosis, while the control group consisted of individuals from the HRS with potential cognitive impairment but no confirmed dementia diagnosis. Unmet social support was characterized by the presence of physical disability in the absence of appropriate assistance. The total population included 1,261 individuals with a dementia diagnosis in the exposure group, and 12,604 individuals with possible cognitive impairment in the control group. Those in the exposure group experienced a significant increase in unmet support for instrumental activities of daily living (IADLs) (coefficient = 0.10, 95% CI [0.07, 0.13]), specifically for help with phone calls (coef = 0.74, 95% CI [0.16, 1.33]). When interpreting the results by race and ethnicity, there was a significant increase in unmet basic activities of daily living (BADLs) (coef = 0.74, 95% CI [0.03, 1.46]) specifically eating difficulties (coef = 1.58, 95% CI [0.17, 2.99]) in Hispanic individuals, and increase in unmet needs for toileting (coef = 1.52, 95% CI [0.57, 2.47]) and IADL support (coef = 0.09, 95% CI [0.00, 0.17]) in Black individuals. By sex, women had fewer unmet BADL (coef = -0.55, 95% CI [-1.03, -0.06]) needs but more unmet IADL support (coef = 0.08, 95% CI [0.04, 0.11]), while men had increased unmet needs for toileting (coef = 0.78, 95% CI [0.03, 1.53] and IADLs (coef = 0.14, 95% CI [0.10, 0.18]). Overall, these results indicate that a dementia diagnosis was associated with an increase in unmet social support, highlighting the need for more equitable care for people living with dementia to prevent the gaps from further increasing.
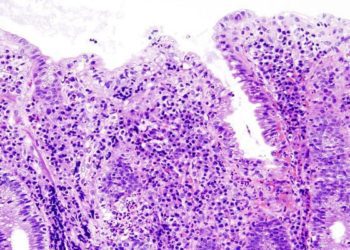
1. In this prospective cohort of fetuses with congenital heart disease (CHD), specifically hypoplastic left heart syndrome (HLHS), a lack of cerebrovascular response to maternal hyperoxia (MH) was associated with smaller brain volume before birth and higher risk of white matter injury after birth.
Evidence Rating Level: 1 (Excellent)
Neurodevelopmental complications are the most frequent coexisting condition in children with significant congenital heart disease (CHD), even with no genetic or other structural abnormalities. Previous studies have suggested that these issues often originate prenatally, since fetuses with CHD show signs of abnormal brain development, including smaller brain volumes and immature brain structure and metabolism. Decreased brain volume is associated with developmental outcomes in infancy and may be a contributor to white matter injury (WMI) after birth, affecting motor outcomes. Predicting neurodevelopmental outcomes before birth remains difficult, limiting the ability to provide targeted counselling and care. One tool that has not been fully explored is maternal hyperoxia (MH) testing, involving administering oxygen to pregnant individuals to affect fetal blood flow. The goal of this study was to investigate whether an abnormal cerebral vascular response to MH testing is associated with poor brain growth and a higher risk of postnatal WMI in fetuses with CHD. The study enrolled 55 participants who underwent a fetal echocardiogram and brain MRI. After adjustments were made, there was no statistically significant association between change in middle cerebral artery pulsatility index (MCA PI) with MH and fetal total brain volume (TBV) (coefficient, 0.21 [95% CI, -0.18 to 0.61]; P=0.28). In fetuses with hypoplastic left heart syndrome (HLHS), those who responded to the oxygen test had, on average, 17.8 mL more TBV than those who had no response, at each week of pregnancy (95% CI, 3.3 to 32.3; P=0.02). This trend was not noted in the d-transposition of the great arteries (D-TGA) group (coefficient, -4.67 [95% CI, -27.0 to 17.61]; P=0.68). Fetuses who developed WMI before surgery showed a significantly lower change in the MCA PI during the oxygen test (mean percentage change, -11.5 [95% CI, -20.5 to -2.6]) compared to those without MI, who showed an average increase of 7.1% (95% CI, -1.9 to 16.2; P=0.04). These results highlight the efficacy and utility of MH testing to help identify fetuses at highest risk for poor neurodevelopmental outcomes.
1. Despite advances in treatment, a cohort of adults from British Columbia, Canda living with HIV (PLWH) continued to experience a higher burden of many physical and mental comorbidities.
Evidence Rating Level: 2 (Good)
Over the past several decades, HIV care has improved drastically; however, comorbidities in people living with HIV (PLWH) have started to burden the healthcare system. These comorbidities often develop at younger ages and with greater severity than in people without HIV (PnLWH). This increased burden is driven by factors such as chronic inflammation, antiretroviral therapy (ART) side effects, and lifestyle factors, among others. This retrospective cohort study aimed to compare trends in physical and mental comorbidities and their related healthcare costs between PLWH and PnLWH. There were 16 physical and mental comorbidities assessed, including major chronic conditions (e.g. cardiovascular disease, diabetes, chronic kidney disease, chronic liver disease, and non-AIDS-defining cancers), neurocognitive disorders, musculoskeletal diseases, and mental health conditions (e.g. mood/anxiety, schizophrenia, personality disorders, and substance use disorder). The study included 9,554 PLWH and 47,770 PnLWH matched based on study criteria. Throughout the study period, PLWH consistently had a higher prevalence of comorbidities even after adjusting for age and sex. Among PLWH, mood disorders were the most prevalent comorbidities, affecting 40% of individuals, compared to 24% in PnLWH. Mental health disorders and substance use disorder (SUD) consistently affected PLWH more than PnLWH. In 2007, PLWH were over 8 times more likely to develop chronic liver disease (CLD) compared to PnLWH (PR=8.30, 95% CI: 6.33 to 10.98). Similarly, in 2008, chronic kidney disease (CKD) was about 6 times more likely to occur in PLWH compared to PnLWH (PR in 2008=6.07, 95% CI: 4.83 to 7.66). The gap in both conditions has narrowed over time, mainly because conditions became less common in PLWH and more common in PnLWH. Healthcare costs were significantly higher in PLWH compared with PnLWH. Despite advances in treatment, PLWH continue to face a higher and evolving burden of comorbidities, particularly mental health disorders and substance use disorder, significantly impacting the healthcare system. This emphasizes the need for comprehensive and integrated care models to better support the complex health needs of PLWH.
Image: PD
©2025 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.