2 Minute Medicine Rewind June 3rd, 2024
Ratio of Red Blood Cell Distribution Width to Albumin Level and Risk of Mortality
1. In this analysis from two prospective cohort studies, an elevated ratio of RDW to albumin concentration (RAR) was found to be independently associated with both all-cause and specific-cause mortality.
Evidence Rating Level: 2 (Good)
Red blood cell distribution width (RDW), a routine laboratory marker measuring the variability in size of circulating erythrocytes, is elevated in instances of impaired erythropoiesis and abnormal red blood cell (RBC) survival, and is associated with mortality as well as other disorders. Serum albumin, on the other hand, is an abundant protein marker that is inversely correlated with nutritional status, disease, and mortality. It has been hypothesized that integrating these two commonly collected biomarkers, represented by the ratio of RDW to albumin concentration (RAR), could predict mortality risk. The current study utilized data from 50,622 participants (mean [SD] age 48.6 [18.7]; 51.6% female; 44.0% White) in the US National Health and Nutrition Examination Survey (NHANES) population-based cohort and 418,950 participants from the prospective, population-based UK Biobank (mean [SD] age 56.6 [8.1]; 53.7% female; 94.3% White) cohort to assess whether elevated RAR was associated with all-cause and specific-cause mortality. This finding was confirmed for participants in the NHANES for all-cause mortality (Hazard Ratio [HR] 1.83, [95% CI, 1.76-1.90]), as well as other disease-specific causes of mortalities, including respiratory disease (HR, 1.99 [95% CI, 1.68-2.35]), malignancy (HR, 1.89 [95% CI, 1.73-2.07]), heart disease (HR, 1.88 [95% CI, 1.74-2.03]), diabetes (HR, 1.55 [95% CI, 1.27-1.90]), cerebrovascular disease (HR, 1.35 [95% CI, 1.07-1.69]), and Alzheimer’s (HR, 1.33 [0.98-1.81]). The findings were amplified for participants in the UK Biobank cohort, with both all cause-mortality (HR, 2.08 [95% CI, 2.03-2.13]) and disease-specific mortality being associated with elevated RAR levels. These findings were significant at all ages (P < .001 for interaction) and despite stratifying for demographics, mental health, chronic disease risk, and socioeconomic status. An additional analysis found that those in the highest quartile of RAR had greater cumulative all-cause and disease-specific mortality than those in the lowest quartiles. Overall, these findings represent the first (and largest) study finding that RAR is independently associated with all-cause mortality in the general population. These results indicate the potential use of RAR as a derived biomarker in routine laboratory testing. Future studies should assess trends in repeated RAR testing as opposed to a single value and account for additional variables not controlled for in the original observational cohort studies.
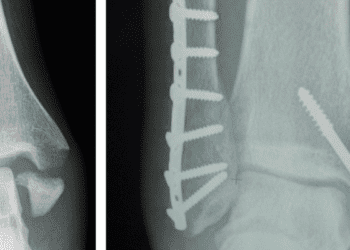
Corticosteroid Injections and Risk of Fracture
1. In a cohort of older adults, the use of corticosteroid injections (CSIs) was not associated with increased fracture risk, regardless of osteoporosis status.
2. The cumulative dose of CSI used over four years was also not a predictor of fracture risk.
Evidence Rating Level: 2 (Good)
Corticosteroid injections (CSI) are commonly used in the management of musculoskeletal (MSK) pain, particularly in older adults. While they are formulated to prolong their presence locally at the injection site, there is some systemic absorption of CSIs. As a result, there is the potential for placing patients at risk for adverse effects of corticosteroids over time, but the extent to which this takes place is not well-studied. One such adverse effect of oral corticosteroids is osteoporosis, which disproportionately impacts older adults and women over the age of 50. The current cohort study sought to elucidate the potential association between cumulative CSI dosing in primary care settings and fracture risk over a four-year span. Patients could have received methylprednisolone, triamcinolone, betamethasone, or dexamethasone injections), and encounter codes for vertebral, wrist, and hip fractures were classified as osteoporotic fractures. Among the 7197 study participants (mean [SD] age, 64.4 [14.6] years; 61.6% women; 92.6% White), 33,684 total CSIs were given mostly in large joints, and the mean (SD) cumulative CSI dose was 141.8 (159.0 [range, 2.7-2140.3]) mg of triamcinolone equivalents. Over the course of the study, 346 patients (4.8%) sustained new fractures, 43.1% of which were in classically osteoporotic regions. On average, a fracture occurred 11 months after the first CSI injection. A further subgroup analysis of high-risk (n = 1845) versus non-high-risk (n = 4741) fracture patients found that 64% of fractures sustained over the course of the study belonged to high-risk patients, and 45% of these fractures were classic osteoporotic fractures. This is in contrast to the non-high-risk group, in which only 22.9% were classic osteoporotic fractures. Also importantly, there was no significant difference in fracture rate between cumulative CSI dose quartiles (5.5% [quartile 1] vs 3.6% [quartile 4]; χ2 P = .87), and both the non-high-risk and osteoporosis subgroups were not found to have associated risk of fracture based on cumulative CSI dose. Only previous fractures, age, and comorbidity were factors associated with fracture risk. These results are the first to comprehensively account for cumulative CSI dosages, and findings indicate that clinicians should not hesitate to prescribe CSIs based on fracture risk, regardless of risk for osteoporosis. The retrospective nature of this study, as well as the homogeneity in race/ethnicity of participants, limit the generalizability of results. Future studies should follow a more diverse cohort of patients over more sustained periods to assess for overall lifetime fracture risk associated with CSIs.
1. Adults with chronic low back pain (CLBP) randomized into a 6-week pain intervention education program were observed to have significantly relieved burden of pain-related disability and overall pain intensity when combined with the physiotherapeutic standard of care.
2. Measures of self-reported well being also improved significantly more in the pain education group compared to the control group.
Evidence Rating Level: 1 (Excellent)
Chronic low back pain (CLBP) is a pervasive condition contributing significantly to pain-related disability worldwide. Several factors are thought to contribute to the burden of CLBP, and pharmacological treatments and physiotherapeutic intervention alone are not believed to be sufficient. The incorporation of psychological strategies and pain education is thought to be crucial, but a lack of standardization and ethnocultural considerations are barriers to widespread implementation. Western countries quite readily embrace pain education programs, and some Eastern countries currently lack robust testing for culturally relevant CLBP curricula. The current randomized controlled trial assessed whether a structured pain education intervention could reduce disability and pain intensity compared to the standard of care. A total of 92 patients with CLBP (mean [SD] age, 42.3 [10.8] years) were recruited from the Sher-e-Kashmir Institute of Medical Sciences (SKIMS) and blindly randomized 1:1 to either the control group or intervention group. Both received 40-minute guideline-based physical therapy sessions, but the intervention group underwent face-to-face education modules exploring definitions of chronic pain, its neurophysiology, and neurobiological aspects (central sensitization, fear avoidance, and social factors affecting CLBP). Didactic sessions occurred twice weekly for the first 3 weeks, followed by question-and-answer sessions in weeks 4 and 5, and a brief education manual was provided at the conclusion of the 6th week. Pain intensity during different activities of daily living (ADLs) was measured on a 0-to-10 scale. Pain-related disability was assessed using the Roland Morris Disability Questionnaire (RMDQ). Measures of self-efficacy and coping were reported using the General Self-Efficacy Scale (GSE), and emotional wellbeing was measured using the World Health Organization (WHO) Five Well-Being Index (WHO-5). Post-intervention results demonstrate that disability burden (RMDQ) scores significantly improved in both groups, but between-group mean difference reflected greater improvements in the experimental group (a 54.2% decrease in disability for experimental group, versus a 6.8% decrease in the control group) with a large effect size (p < .001, Cohen’s d = 0.75). Pain intensity decreased in both groups, with significant main effect and large effect size between the groups post-intervention (p < 0.001, Cohen’s d = 0.82). Measures of well-being on the WHO-5 improved in favor of the pain education group, with a moderate effect size (p < 0.001, Cohen’s d = 0.58). Scores on the GSE scale were not affected by the treatment. A regression found that higher reports of RMDQ at baseline were associated with elevated disability at 6 weeks, and higher educational attainment was protective against disability post-intervention. Higher pain scale scores increased the odds of high pain intensity at 6 weeks by 1.69-fold, and higher self-efficacy, female sex, and higher age at baseline were associated with positive outcomes for well-being and self-efficacy. Overall, results suggest that integrating a pain education program with standard physiotherapeutic care enhanced outcomes for CLBP patients in India, and multi-centre trials should be conducted to improve the external validity of results.
1. In this randomized, double-blind, placebo-controlled trial, the use of once-weekly subcutaneous TG103 resulted in significant weight reduction at 12 weeks at all dosages.
2. It was deemed to be safe and effective, with pharmacokinetic findings in keeping with the weekly dose regimen recommended in preclinical studies.
Evidence Rating Level: 1 (Excellent)
Obesity, caused by complex interactions between behavioural, environmental, genetic, metabolic, and neuroendocrine factors, is the most prevalent chronic disease worldwide. It is associated with a greater burden of comorbidity, disability, and mortality, as well as economic strain on the healthcare system. While various interventions, including lifestyle modifications, behavioral therapies, and surgical procedures, are available, pharmacological treatments such as glucagon-like receptor agonists (GLP-1 RAs) are increasingly recognized for their potential in providing sustainable drug-based management of obesity. Despite the approval of several GLP-1 RAs for obesity treatment in the United States, none are approved for use in China, highlighting unmet medical needs in this population. TG103 is a recombinant protein exhibiting an affinity for the GLP-1 receptor with a long half-life, making it a possible candidate for weekly injections in the treatment of obesity. The current randomized, double-blind, placebo-controlled, multiple-dose phase 1b study investigated the safety, pharmacokinetics, and tolerability of weekly subcutaneous TG103 injection for nondiabetics in China. A total of 48 nondiabetic overweight or obese adults (mean [SD] age, 33.9 [10.0] years; mean [SD] weight, 81.65 [10.5] kg; mean BMI 29.8 kg/m2) were assigned to one of three groups (n = 16). Within each group, 12 were randomly assigned to receive TG103 and 4 were assigned to receive the placebo. Group A TG103 participants received 7.5 mg in week 1, followed by 15 mg for the remaining 11 weeks. Group B received 7.5 mg, followed by 15.0 mg, and then 22.5 mg from weeks 3-12. Group C TG103 participants received 7.5 mg, 15.0 mg, 22.5 mg, followed by 30 mg from weeks 4-12. While there were adverse events (AEs) recorded in 45 of the 48 participants (97.2% of TG103 patients and 83.3% of placebo patients), no serious AEs occurred. AEs in the TG103 group included: decreased appetite (58.3%), nausea (55.6%), diarrhea (52.8%), injection-site reaction (47.2%), hypertriglyceridemia (33.3%), vomiting (33.3%), and hyperuricemia (22.2%). Decreased appetite and gastrointestinal disturbances including vomiting, diarrhea, and abdominal distention were found to be dose-dependent. From a pharmacokinetic standpoint, the time to maximum concentration (Tmax) was 36.0, 35.8, and 48.0 hours for the 15 mg, 22.5 mg, and 30 mg target doses. In all groups, the blood concentration of TG103 stabilized by the 10th dose. The incidence of antibodies to TG103 was 22.2%. Mean weight change from baseline by day 85 was 5.65 kg (Group A; 7.24% loss), 5.35 kg (Group B; 5.79% loss), and 5.13 kg (Group C; 6.47% loss), whereas the placebo group lost only 1.37 kg from baseline. The placebo and experimental groups both saw decreases in waist circumference and waist-to-hip ratios, but did not differ significantly from one another. Systolic blood pressure (SBP) decreased the most in Group C, followed by Group B. There were no differences between Group A and placebos in SBP. To conclude, all three doses of once-weekly TG103 were well tolerated with acceptable GLP-1 RA safety profiles and pharmacokinetic parameters supporting the once-weekly dosing. Future trials are required to fully elucidate the efficacy and safety profile of TG103.
1. In this retrospective analysis, compared to nonsmokers, vaping (both within the previous month and at all in the past) was associated with increased incidence of respiratory symptoms.
2. The use of nicotine salts and fruit-flavoured vapes were also associated with increased odds of self-reported respiratory symptoms.
Evidence Rating Level: 2 (Good)
Within the past ten years, the use of vapes has increased among US, Canadian, and British adolescents, whereas the prevalence of cigarette smoking has decreased or remained relatively unchanged. While switching from cigarettes to vaping reduces health risks, the use of vapes among adolescents and those who are not previous smokers presents potential risks associated with exposure to ultrafine particles and constituents in vape aerosols. The current study’s aim is to assess self-reported respiratory symptoms in young people from the aforementioned countries. Data from participants (n = 39,214; ages 16 to 19; 65% White, 51.6% male) of the International Tobacco Control Policy Evaluation Project (ITC) Youth Tobacco and Vaping Surveys (Canada, England, US) were included in analyses. Participants were surveyed on their smoking/vaping behaviours within the past 30 days and within their lifetime. They were also asked to self-report for any of the following five respiratory symptoms: shortness of breath, wheezing, chest pain, phlegm, or cough. Within the past 30 days at the time of surveying, most had not smoked or vaped (82.8%), under 3% had smoked or vaped on at least 20 days, and nearly one-fifth reported using at least one other inhaled product (most commonly cannabis) in the past month. Results indicated that over one-quarter (27.8%) of surveyed adolescents reported any of the five respiratory symptoms within the past 7 days (cough was the most common). There were similar odds of experiencing respiratory symptoms between those who only vaped and those who only smoked [adjusted odds ratio, aOR (95% CI): 0.97 (0.85–1.10)], and higher odds if participants both smoked and vaped [aOR (95% CI) 1.26 (1.12–1.42)]. Compared to those who never smoked or vaped, any past use, experimentation, or current regular or occasional use of vapes was associated with increased odds of respiratory symptoms. Those who vaped on at least 20 of the last 30 days were most likely to report respiratory symptoms, with each additional day associated with an increase in odds of developing symptoms (p < .001). The use of nicotine salts and certain vape flavours were also associated with the highest odds of respiratory symptoms, including fruit [1.44 (1.07–1.93)], multiple [1.76 (1.30–2.39)] and ‘other’ [2.14 (1.45–3.16)]. Tobacco, menthol, and mint flavours were nonsignificant, and the type of vaping device used (pre-filled cartridge, pod, disposable, etc.) did not significantly impact the incidence of respiratory symptoms. Overall, in this international cohort of adolescents, vaping was associated with higher odds of self-reporting respiratory symptoms within the last week and odds increased with increased frequency of vaping.
Image: PD
©2024 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.