Delayed antibiotic prescribing for respiratory infections may decrease unnecessary antibiotic use
1. In this randomized controlled trial, delayed antibiotic prescribing strategies resulted in decreased antibiotic use.
2. Patients in the delayed prescription or no antibiotic groups reported longer duration of moderate to severe symptoms as compared to the immediate antibiotic group. However, no placebo group existed for complete comparison.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Many upper respiratory illnesses in ambulatory patients are due to viruses, and therefore antibiotics have limited use. In primary care, where there may be higher diagnostic uncertainty, delayed antibiotic prescribing strategies have been suggested to reduce unnecessary antibiotic use. This open-label randomized controlled trial aimed to determine the efficacy and safety of two delayed antibiotic strategies in acute uncomplicated respiratory infections as compared to immediate antibiotic prescription or no offer of antibiotics.
The two delayed antibiotic prescribing strategies resulted in decreased antibiotic use. Patients in the delayed antibiotic and no antibiotic groups, however, had a longer duration of symptoms self-reported as moderate-to-severe than those with immediate prescriptions. Overall, patient satisfaction was high and similar across all groups. While this is a randomized controlled trial, a major limitation to this study is the lack of a placebo group. There may be a component of bias as well, given all data is based on self-reported daily questionnaires.
Click to read the study, published today in JAMA Internal Medicine
Relevant Reading: Delayed antibiotics for respiratory infections
In-Depth [randomized controlled trial]: This open-label, randomized controlled trial was conducted between December 2009 and July 2012 in 23 primary care centers in Spain. Eligible patients were adults with acute uncomplicated respiratory infections (acute pharyngitis, rhinosinusitis, acute bronchitis, COPD exacerbation). Patients were randomized to four treatment strategies: immediate prescription, no prescription, patient-led prescription (patients are given prescription on first consultation), and prescription collection strategy (patients collect the antibiotic at primary care office after the consultation). Both delayed strategy groups were told the same criteria on when to use or come back for antibiotics. The primary outcome of interest was duration and severity of symptoms as measured by daily self-reported questionnaires. Secondary outcomes included antibiotic use, satisfaction with health care, and absenteeism.
A total of 405 patients were recruited, and 398 included in analysis, which were primarily non-smokers without respiratory comorbidity. The duration of self-reported moderate symptoms in the immediate antibiotic group was statistically shorter and had a mean of 4.7 days (SD 4.0) as compared to 5.2 days (4.3), 6.0 days (5.5) and 6.5 days (5.2) in the collection, patient-led, and no prescription groups, respectively (p < 0.001). There was a similar pattern for severe symptoms (p = 0.002). The only individual symptom that had a significantly longer duration in the delayed or no prescription group was discomfort or general pain (p = 0.002). In the delayed strategies groups, only 23% and 32% of the collection and patient-led groups used antibiotics as compared to 92% of the immediate antibiotic group. Absenteeism was lower in both delayed groups (21.4% in prescription collection, 25.8% in patient-led) as compared to the higher rates in the immediate prescription group and no prescription group (33.3% and 39.8% respectively; p = 0.05).
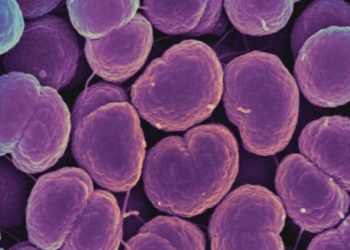
Image: CC/Wiki
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.



![Oral amoxicillin as effective as injectable benzylpenicillin-gentamicin for infants with infection in which referral not possible [AFRINEST Trial]](https://www.2minutemedicine.com/wp-content/uploads/2015/04/NOVAMOXIN_antibiotic-350x250.jpg)


