Hemodynamic-guided management of heart failure may reduce hospitalization rates
1. In the pre-COVID-19 analysis, hemodynamic monitoring reduced hospitalization and all-cause mortality rates.
2. After the COVID-19 pandemic started, hospitalization of heart failure patients was reduced and there were no appreciable differences between the control and hemodynamic monitoring group.
Evidence Rating Level: 1 (Excellent)
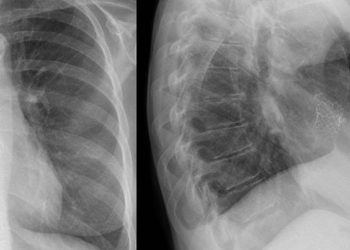
Study Rundown: Worsening hemodynamic congestion is a major cause of hospitalization in patients with heart failure. Hemodynamic congestion may be measured by raised pulmonary artery pressure as an indicator of left atrial pressure. In the GUIDE-HF study, pulmonary artery pressure was measured by an inserted monitor in all 1000 participants with heart failure. In this study, half the patients were randomized to have their treatment decisions be guided by the pulmonary artery pressure, while the other half received usual care. The primary outcome was a composite measure of all-cause mortality and hospitalization events. Unfortunately, this study was impacted by the COVID-19 pandemic as hospitalization rates were greatly affected. Consequently, results were split into pre-COVID-19 and overall outcome events. Pre-COVID-19, hemodynamic monitoring appeared to lower rates of hospitalization and mortality compared to usual treatment. However, this difference was diminished after the start of the pandemic. While the rate of events of the hemodynamic group did not change after the start of the pandemic, the hospitalization rate of the control group decreased by 21%. The pandemic may have lowered the chance that patients would go to the hospital or get admitted and therefore affected the results of this study. Nonetheless, the results pre-pandemic showed promise despite only being for a few months.
Click to read the study in the Lancet
In-Depth [randomized controlled trial]: GUIDE-HF is a single-blind randomized control trial that took place in the USA and Canada. Heart failure patients were randomized 1:1 to either a hemodynamic-guided heart failure or treatment as usual. All 1000 patients had a pulmonary artery pressure monitor implanted, but only the hemodynamic group had it used to guide management decisions. Investigators did not have access to pulmonary artery pressure from the control patients. The primary outcome was all-cause mortality and total heart failure events (hospitalization). The trial lasted 12 months and 38% of the participants were female.
This study reported results depending on if the outcomes occurred pre-COVID or after the start of the pandemic. In the overall cohort analysis, there were no differences in all-cause mortality and hospitalization between the hemodynamic-guided management group and the control group (HR 0.88, 95% CI 0.74-1.05, p=0.16). However, pre-COVID-19 analyses demonstrated fewer primary events in the hemodynamic-guided management group (0.553 per patient year) compared to the control group (0.6682 per patient year; HR 0.81 [95% CI 0.66-1.00]; p=0.049). Post-COVID, the difference in risk diminished to a ratio of 1.11 (95% CI 0.80-1.55, p=0.53). The occurrence of serious adverse events were similar between the hemodynamic-guided management group (57%) and the control group (53%).
Image: PD
©2021 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.