Human papillomavirus infection is associated with adenocarcinoma of the cervix [Classics Series]
This study summary is an excerpt from the book 2 Minute Medicine’s The Classics in Medicine: Summaries of the Landmark Trials
1. Human papillomavirus (HPV) types 16 and 18 were present in a high proportion of cervical disease and termed oncogenic subtypes.
2. Infection with HPV subtypes 16 or 18 conferred at least a 60-fold increased risk of developing cervical cancer.
Original Date of Publication: March 1992
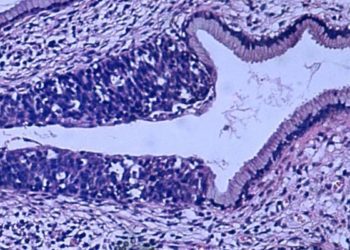
Study Rundown: HPV was first linked to cervical cancer in the early 1980s. Since that time, molecular biologists worked to better understand the relationship between HPV exposure, infection and cervical cancer. Regarding exposure and infection, studies demonstrated variable association with exposure and subsequent persistent HPV infection. With respect to cervical cancer, a large investigation demonstrated that HPV strains 16 and 18 were present in 70% of all cervical cancer specimens, suggesting these 2 strains were associated with development of dysplasia and cancer. Other HPV serotypes were detected in low-risk cervical pathology but were much less frequent. Thus, the proportion of women exposed to HPV who would develop persistent infection and of those, the proportion who would develop cervical cancer, remained unclear.
In this landmark work, authors assessed the incidence of HPV in healthy controls, the clinicopathologic relationship of 15 common HPV strains, and condylomatous, premalignant, and malignant cervical disease. Authors determined that the HPV subtypes 16, 18, 45 and 56 were the most commonly found subtypes in cervical dysplasia and neoplasia. Additional novel findings included a frequency (6%) of HPV infection in the normal population, which was remarkably low considering the frequency with which women are exposed. Strengths included a large sample size with over 2500 subjects and blinding of scientists performing HPV probes to the clinical cervical diagnoses. Limitations included secondary analysis, case-control study design, and use of a convenience sample which may subject findings to selection or recall bias.
Click to read the study in Obstetrics & Gynecology
In-Depth [randomized controlled trial]: A total of 2627 women previously recruited into the studies performed at Life Technologies on HPV infection and cervical neoplasia study submitted to retesting of previously-collected 731 biopsy specimens and 1896 cervical swabs for HPV testing for the most common 15 subtypes. Controls were defined as healthy (normal) and cases were defined as condyloma, premalignant, or invasive/malignant cervical disease by final surgical pathology. The primary exposure of interest was infection with each of the most common 15 HPV subtypes and cervical disease. The incidence of HPV infection in each patient group was assessed and outcomes included continued healthy status, borderline atypia, low-grade squamous intraepithelial lesion (LSIL), high-grade squamous intraepithelial lesion (HSIL), and cancer. Data were presented as relative risk values, which were estimated from odds ratios.
HPV infection was detected in 79% of women with cervical dysplasia or neoplasia, 24% of women with borderline atypia, and 6% of normal subjects. Multiple HPV risk categories were identified: high-risk, or oncogenic, subtypes 16 (present in 47% of HSIL and 47% of cancers) and subtypes 18 (in 7% of HSIL and 27% of cancers), intermediate-risk types 31, 33, 35, 51, 52, 58 (in 24% of HSIL and 11% of cancers), and low-risk subtypes 6, 11, 42, 43, 44 (in 0% of cancers and 20% of LSIL). The relative risk of cervical disease associated with oncogenic HPV subtypes ranged from 65-236 for cervical cancer and 31-296 for high-grade dysplasia.
Lorincz AT, Reid R, Jenson AB, Greenberg MD, Lancaster W, Kurman RJ. Human papillomavirus infection of the cervix: relative risk associations of 15 common anogenital types. Obstetrics and gynecology. 1992;79(3):328-37.
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc