Letrozole superior to clomid for ovulation induction in PCOS [Classics Series]
1. Women with polycystic ovary syndrome (PCOS) randomized to receive letrozole had more live births than women randomized to clomiphene (27.5% vs. 19.1%, p=0.007).
2. Cumulative ovulation rates were higher in women on letrozole compared to those on clomiphene (61.7% vs. 48.3%, p<0.001).
Original Date of Publication: July 2014
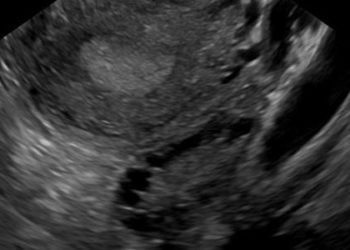
Study Rundown: Polycystic ovary syndrome (PCOS) affects 5-10% of women in the United States and is the most common cause of ovulatory disorders. The diagnosis requires anovulation or oligoovulation as well as either signs of hyperandrogenism or songoraphic evidence of polycystic ovaries (12+ follicles sized 2-9mm in each ovary and/or increased ovarian volume >10 mL). By definition, women with PCOS do not spontaneously ovulate each month such that fertility treatments, specifically, ovulation induction, is often required for conception. The most commonly used agent for ovulation induction in PCOS is clomiphene citrate (clomid), an estrogen receptor antagonist that increases endogenous gonadotropins (follicle-stimulating hormone and luteinizing hormone) to prevent estrogen’s negative feedback on the hypothalamus. Insulin resistance, another feature of PCOS, is treated with metformin. Previous studies evaluated whether meformin may improve live birth rates when used either alone or in combination with clomid (see relevant reading). Results demonstrated that metformin alone or in combination with clomid was no better than clomid alone. Aromatase inhibitors disrupt the hypothalamic-pituitary-ovarian axis by blocking estrogen synthesis and therefore might allow a more physiologic stimulation of the ovaries and endometrium thereby improving live birth rates. In the present study, researchers randomized women to receive either clomid or the aromatase inhibitor letrozole for ovulation induction and found that letrozole resulted in more live births.
This landmark study demonstrated that women with PCOS have a higher number of live births on letrozole compared to clomid such that practice is now shifting to offer these women letrozole instead of clomid. Strengths of this investigation include an elegant randomized controlled design and examination of delivery, birth and neonatal records for all live births. Limitations included drop-out rate of 20% and a larger proportion of obese patients such that results may be biased and may not apply to women with lean PCOS. While a multi-center design is a strength of this investigation, certain practices (e.g. inducing a withdrawal bleed after anovulatory cycles) varied by fertility center and created an opportunity for bias.
Click here to read study in NEJM
Relevant reading: Clomiphene, metformin, or both for infertility in the Polycystic Ovary Syndrome 2003 Rotterdam Criteria
In-Depth [randomized controlled trial]: A total of 750 women with polycystic ovary syndrome were randomized to receive either clomiphene (n=375) or letrozole (n=375) for up to five ovulation induction cycles in this double-blinded, multicenter RCT conducted through the Reproductive Medicine Network. Women aged 18-40 years with a diagnosis of PCOS (anovulation or oligoovulation with hyperandrogenism or polycystic ovaries), a normal uterine cavity and at least one patent fallopian tube were eligible. Women with partners with male factor infertility were excluded. Couples engaged in regular and/or timed intercourse and the primary outcome of live birth was assessed.
Among women with PCOS, those randomized to letrozole experienced more cumulative live births than those randomized to clomiphene (27.5% vs. 19.1%, p=0.007). Women on letrozole also experienced higher cumulative ovulation rates (61.7% vs. 48.3%, p<0.001). There were no significant differences in the incidences of pregnancy loss, twin pregnancy or birth defects. Rates of adverse effects were similar between treatment groups aside from a higher incidence of hot flushes with clomiphene and fatigue and dizziness with letrozole.
Image: PD
More from this author: HPV triage is optimal management for ASCUS [Classics Series], Risks of trial of labor after cesarean delivery (TOLAC) [Classics Series], Vaginal progesterone for sonographic short cervix decreased preterm birth [Classics Series]
©2014 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. No article should be construed as medical advice and is not intended as such by the authors, editors, staff or by 2 Minute Medicine, Inc.