Pantoprazole prophylaxis for individuals on mechanical ventilation with stress ulcers
1. In this randomized controlled trial studying critically ill adults, pantoprazole use was associated with a lower risk of clinically important upper gastrointestinal bleeding compared to placebo use.
2. There was no significant increase in C. difficile infection, pneumonia infection, or mortality in the pantoprazole group compared to the placebo group.
Evidence Rating Level: 1 (Excellent)
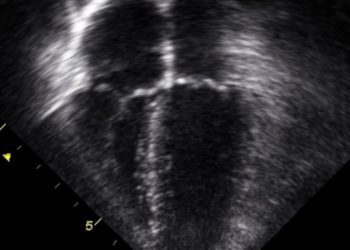
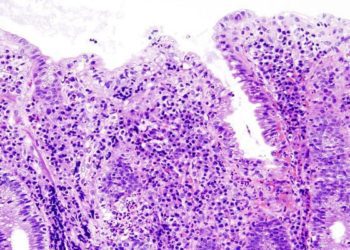
Study Rundown: Individuals with a chronic illness are at a higher risk of developing stress-induced gastrointestinal ulcerations, possibly leading to gastrointestinal bleeding. To assess the effects of proton pump inhibitors on stress ulcer prophylaxis, the study enrolled patients in the Reevaluating the Inhibition of Stress Erosions (REVISE) trial. This randomized controlled trial was conducted across 68 hospitals worldwide. The eligible participants were randomized in a 1:1 ratio to receive the placebo or intravenous pantoprazole. To ensure complete blinding, the coloring of the placebo and pantoprazole matched, and the nurses who knew the groupings were the ones who prepared the pantoprazole (40 mg reconstituted with 0.9% sodium chloride) and the matching placebo (0.9% sodium chloride). Blinded staff members administered the dose to each participant for 90 days or until the invasive ventilation was stopped. The main outcome was clinically important upper gastrointestinal bleeding at 90 days, while the main safety outcome was all-cause mortality at 90 days. Since all the patients in the study were supported by mechanical ventilation, it is unclear whether the findings would apply to patients with unassisted breathing. In summary, pantoprazole decreased the risk of clinically important upper gastrointestinal bleeding compared to the placebo in a cohort of individuals on mechanical ventilation.
Click to read the study in NEJM
In-Depth [randomized controlled trial]: A blinded randomized controlled trial was initiated to determine the efficacy of pantoprazole compared to placebo in treating stress ulcers in critically ill adults being mechanically ventilated. Those eligible to participate had to be 18 years or older and undergo invasive mechanical ventilation in the ICU, which was expected to continue until at least the day after randomization. Exclusion criteria also indicated that individuals who were started on invasive ventilation in the ICU 72 hours or more before randomization or had received more than one dose equivalent of acid suppression daily were not eligible. During randomization, the 4,821 participants were split into two groups, with 2,417 assigned to the pantoprazole group and 2,404 to the placebo group. Clinically important upper gastrointestinal bleeding was more prevalent in the placebo group as 84 of 2,377 patients (3.5%) receiving placebo had it, whereas 25 of 2,385 patients (1.0%) in the pantoprazole group had it (hazard ratio, 0.30; 95% confidence interval [CI], 0.19 to 0.47; p<0.001). Mortality occurred in 29.1% (696 of 2,390) of the patients in the treatment group and 30.9% (734 of 2,379) of patients in the placebo group (hazard ratio, 0.94; 95% CI, 0.85 to 1.04; p=0.25). Of the 2,394 patients in the pantoprazole group, 556 (23.2%) experienced ventilator-assisted pneumonia, whereas this occurred in 567 of the 2,381 patients (23.8%) in the placebo group. C.difficile affected fewer participants, with only 28 of 2385 (1.2%) individuals and 15 of 2377 (0.7%) of individuals in the pantoprazole and placebo groups, respectively. In summary, patients receiving pantoprazole did not have an increased risk of developing ventilator-associated pneumonia or C. difficile infection compared to patients receiving the placebo.
Image: PD
©2024 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.