Premorbid neurodegenerative disease associated with increased risk of COVID-19 infection and death
1. Premorbid neurodegenerative disease was linked to a significantly increased risk of COVID-19 infection and death.
2. Among patients with neurodegenerative diseases, vascular etiology may increase COVID-19 risk compared with primary causes.
Evidence Rating Level: 2 (Good)
Study Rundown: Chronic diseases and multimorbidity have been associated with more severe COVID-19 disease courses. Several cohort studies have investigated association of neurodegenerative diseases with poorer prognosis for COVID-19 infection, but evidence to date is inconclusive. This retrospective cohort study aimed to assess association between neurodegenerative diseases and risk of COVID-19 infection. Using an English cohort, the study reported on COVID-19 outcomes in participants who received nucleic acid tests before June 14, 2021. The outcomes of interest included COVID-19 diagnosis, inpatient COVID-19 and COVID-19 related death. A total of 96,275 patients, of which 2,617 (2.7%) had neurodegenerative diseases, were included. Separate analyses were completed for patients with COVID-19 infection during 4 consecutive time periods and different neurodegenerative disease course stages, to account for dominant virus strains and comorbid illness severity, respectively. Within this cohort, 17,938 individuals (18.6%) had COVID-19, with 5749 inpatient cases and 1181 COVID-19 related deaths. Individuals with comorbid neurodegenerative disease had significantly increased risk of any COVID-19 infection across all time periods, in addition to increased risk of inpatient admission and deaths. Overall, this provides evidence that neurodegenerative comorbidities are associated with worse COVID-19-related outcomes and consideration of current screening and prevention practices in these patient populations may be important. Notably,
Click here to read the study in BMC Neurology
Click to read an accompanying editorial in Journal of Parkinson’s Disease
Relevant Reading: Resilience of Alzheimer’s Disease to COVID-19
In-Depth [Retrospective cohort study]: This study included 96,275 patients from a large prospective cohort, UK Biobank, which recruited 502,507 participants from ages 40-69 years between 2006 and 2010. Mortality data was collected from several death registers, including but not limited to NHS digital (England and Wales) and NHS central register (Scotland). Results of COVID-19 nucleic acid tests were received from Public Health England (PHE) which were also linked to UK Biobank with monthly updates.
To account for differences in association across dominant virus strains and testing methods, separate analyses were calculated for the time periods before April 26, 2020, April 27 2020 to July 6 2020, July 7 2020 to December 16 2020, and December 17 2020 to June 14 2021. Somatic comorbidities were considered confounds and assessed using the Charlson Comorbidity Index. It was found that there was an elevated risk of COVID-19 infection observed in patients with neurodegenerative disease compared to those without (27.4% vs. 18.4%), as well as increased risk of inpatient admission (14.5% vs 5.7%) and COVID-19 associated death (7.5% vs 1.1%). Neurodegenerative disease was associated with an increased risk of COVID-19 infection [OR 2.47 (95% CI 2.25-2.71)], inpatient COVID-19 admission [OR 2.18 (95% CI 1.94-2.45)] and COVID-19 related death [OR 3.67 (95% CI 3.11-4.34)]. This risk was more pronounced for individuals with vascular neurodegenerative diseases compared with primary etiologies, OR 4.79 (95% CI 3.84-5.97, p <0.001). A positive association between infection and neurodegenerative disease diagnosis was also found across all studied time periods (OR 1.49 [95% CI 1.13-1.97]) before April 26 2020, OR 4.00 [95% CI 3.11-5.15] from April 27 2020-July 6 2020, OR 1.72 [95% CI 1.47-2.01] during July 7 2020-December 16 2020, and OR 2.52 [95% CI 2.15-2.96] from December 17 2020 to June 14 2021. Moreover, sensitivity analysis was performed in order to remove the potential confound of age as a risk factor for both neurodegenerative disease and severe COVID-19 infection. All patients with neurodegenerative diseases were compared with 5 age- and sex-matched individuals without such diseases who were randomly selected from the study population. Following sensitivity analysis, findings were similar to the original study, with OR 2.17 (95% CI 1.96-2.41) for any COVID-19 infection [OR 2.17 (95% CI 1.89-2.48)] for inpatient COVID-19 and OR 3.90 (95% CI 3.17-4.79) for COVID-19 related death.
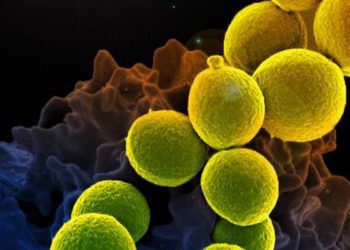
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.