Type 2 diabetes and abnormal amyloid concentrations are associated with accelerated brain atrophy
1. Type 2 diabetes and abnormal amyloid-β concentration (low Aβ42:Aβ40 ratio) in the cerebrospinal fluid were associated with accelerated brain atrophy and earlier progression from normal cognition to mild cognitive impairment in middle-aged and older adults.
Evidence Rating Level: 2 (Good)
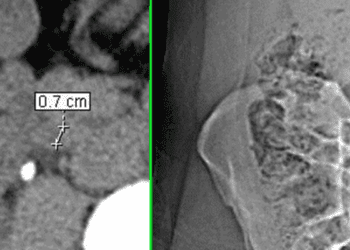
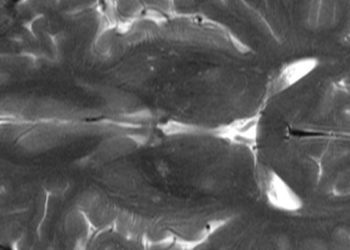
Study Rundown: The lack of longitudinal brain magnetic resonance imaging (MRI) data over 10 years limits the understanding of the risk factors that accelerate brain atrophy and cognitive decline over time. This longitudinal study therefore investigated the risk factors for the acceleration of brain atrophy and progression from normal cognition to MCI) in middle-aged and older adults. This study analyzed data from the Biomarkers for Older Controls at Risk for Dementia (BIOCARD), which included individuals who were cognitively normal at baseline and were followed for an average of 20.2 (±3.0) years. Participants were included in this study if they had structural brain MRI and cerebrospinal fluid (CSF) measurements available for over 10 years. A total of 185 participants aged 20-76 years at baseline were included and followed up for a maximum of 27 years. During the follow-up period, 60 participants progressed to MCI. Participants with type 2 diabetes and those with a low CSF ratio of amyloid β peptide 42 (Aβ42) to Aβ40 (Aβ42:Aβ40) showed higher annual change in white matter atrophy and ventricular enlargement over time compared to those without diabetes and with a high Aβ42:Aβ40 ratio, respectively (p < 0.05). Greater differences were found for participants with a combination of type 2 diabetes and low Aβ42:Aβ40 ratio compared to those with one risk factor (p < 0.05). Participants with high levels of white matter atrophy and ventricular enlargement had an earlier progression from normal cognition to MCI symptom onset. Additionally, progression from normal cognition to MCI was associated with type 2 diabetes and low CSF Aβ42:Aβ40 ratio, and their combined presence was associated with a greater risk. Overall, this study found that higher rates of change in brain volume, along with the presence of type 2 diabetes and a low CSF Aβ42:Aβ40 ratio were important risk factors for the progression from normal cognition to MCI in middle-aged and older adults. Identifying individuals with these risk factors may help guide appropriate interventions to prevent or slow their progression to MCI.
Click to read the study in BMC Medicine
Relevant reading: The Association of Late-Life Diabetes Status and Hyperglycemia With Incident Mild Cognitive Impairment and Dementia: The ARIC Study
In-Depth [Retrospective cohort study]: This longitudinal cohort study investigated risk factors for the acceleration of brain atrophy and progression from normal cognition to MCI in middle-aged and older adults. This study analyzed data from the Biomarkers for Older Controls at Risk for Dementia (BIOCARD), which included individuals who were cognitively normal at baseline and followed for an average of 20.2 (±3.0) years with clinical and cognitive assessments, brain MRI scans, and CSF measures of Alzheimer’s biomarkers. BIOCARD was initiated at the National Institutes of Health (January 1, 1995 – December 31, 2005) and continued at Johns Hopkins University (January 1, 2015, to October 31, 2023). Participants with structural brain MRI and CSF measures available for over 10 years were included. A total of 185 participants aged 20-76 years at baseline (mean [SD] age, 55.4 [8.4] years; 116 women [63%]) were included and followed up for a maximum of 27 years (median, 20 [IQR, 18-22] years). During the follow-up period, 60 participants progressed to MCI (mean [SD] age, 57.2 [8.9] years; 36 women [60%]). The total number of MRI scans was 951, with a median of 5 scans per participant (IQR, 4-6). Participants with type 2 diabetes and those with a low CSF Aβ42:Aβ40 ratio showed higher annual change in white matter atrophy and ventricular enlargement over time compared to those without diabetes and those with a high Aβ42:Aβ40 ratio, respectively (p < 0.05). Greater differences were found for participants with a combination of type 2 diabetes and low Aβ42:Aβ40 ratio compared to those with one risk factor (p < 0.05). Annual change rates of the brain volumes were not associated with other vascular risk factors (hypertension, dyslipidemia, smoking) or CSF biomarkers (p-tau181 and t-tau). Earlier progression from normal cognition to MCI symptom onset was observed for participants with high levels of white matter atrophy (Hazard ratio (HR), 1.86 [95% CI, 1.24- 2.49]) and ventricular enlargement (HR, 1.71 [95% CI, 1.19-2.24]). Additionally, progression from normal cognition to MCI symptomatic onset was associated with type 2 diabetes (HR, 1.41 [95% CI, 1.06-1.76]) and low CSF Aβ42:Aβ40 ratio (HR, 1.48 [95% CI, 1.09-1.88]), and their combined presence was associated with a greater risk (HR, 1.55 [95% CI, 1.13-1.98]). Overall, this study found that higher rates of change in the white matter and ventricle volumes, as well as the presence of type 2 diabetes and low CSF Aβ42:Aβ40 ratio were important risk factors for the progression from normal cognition to MCI middle-age and older adults. A synergic association may exist between type 2 diabetes and amyloid pathology with MCI progression. Future longitudinal studies with larger sample sizes are warranted to confirm study findings. Identifying individuals with risk factors for brain atrophy and cognitive decline is important for developing targeted interventions to prevent or slow their progression from normal cognition to MCI.
Image: PD
©2025 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.