Uninterrupted warfarin therapy safe for endovascular procedures
1. Meta-analysis suggests that there is no difference in risk of access site hematoma, bleeding complication, or mortality between interrupted and uninterrupted warfarin therapy for arterial endovascular procedures.
2. For venous procedures, uninterrupted warfarin therapy was associated with a decreased risk of access site hematoma or bleeding complications, and secondary estimates of thrombosis rates were decreased relative to interrupted warfarin therapy as measured by risk of ischemic stroke or myocardial infarction.
Evidence Rating: 2 (Good)
Study Rundown: Patients at risk for thromboembolism, most commonly secondary to atrial fibrillation, on chronic anticoagulation with warfarin commonly discontinue anticoagulation temporarily for endovascular procedures. During this interval off anticoagulation prior to the procedure, patients run a theoretical risk of developing a new thrombosis causing an ischemic stroke, pulmonary embolism, or myocardial infarction if their warfarin is stopped which is weighed against an increased risk of periprocedural bleeding if their anticoagulation is continued. This systematic review and meta-analysis aimed to investigate the risk of bleeding, access site hematoma, and mortality following both arterial and venous endovascular procedures in patients with and without interrupted warfarin therapy.
There was no significant difference between uninterrupted and interrupted warfarin therapy in access site hematoma, bleeding complications, ischemic stroke, or major bleeding when pooling both arterial and venous procedures, and risks of ischemic stroke, major bleeding and access site hematoma actually were reduced among patients undergoing uninterrupted warfarin therapy prior to venous procedures. A lower risk of thrombotic events was attributed to continued anticoagulant therapy, while the decreased risk of bleeding was attributed to the risk provided by bridging patients wherein overlapping agents may provide supratheraputic anticoagulation. This study suggests that arterial and venous endovascular procedures are safe to perform concurrently with warfarin anticoagulation, and that uninterrupted therapy may in fact be associated with superior patient outcomes when performing venous procedures. This study was limited in that few included studies were high-quality randomized controlled trials, no examination of novel oral anticoagulants were included, and concomitant antiplatelet therapy was not assessed, nor were differences in puncture site or use of bridging therapy between anticoagulants. Future studies should aim at providing prospective controlled data to evaluate safety and efficacy, and expand data to include novel oral anticoagulants, antiplatelet agents and different types of endovascular procedures.
Click to read the study in Journal of Radiology
In-Depth [meta-analysis]: A literature search of papers from 1990-2014 was completed. Reports comparing vascular procedures in patients on chronic warfarin anticoagulation were included, with 27 studies and a total of 20 376 patients found. In arterial procedures, there was no difference between interrupted and uninterrupted warfarin therapy in access site hematoma (OR, 0.59; 95% confidence interval [CI]: 0.33, 1.03; p = 0.06), any bleeding complications (OR, 0.56; 95% CI: 0.30, 1.06; p = 0.07), mortality (OR, 1.40; 95% CI: 0.37, 5.25; p = 0.62), intracranial hemorrhage (OR, 0.55; 95% CI: 0.03, 8.91; P = .68), ischemic stroke (OR, 0.85; 95% CI: 0.12, 5.84; p = 0.87), and major bleeding (OR, 0.56; 95% CI: 0.21, 1.51; p = 0.25). For venous procedures, uninterrupted warfarin was associated with lower odds of access site hematoma (OR, 0.70; 95% CI: 0.50, 0.99; p = 0.04), any bleeding complications (OR, 0.61; 95% CI: 0.48, 0.77; p < 0.01), ischemic stroke (OR, 0.21; 95% CI: 0.10, 0.45; p < 0.01), and major bleeding (OR, 0.64; 95% CI: 0.51, 0.80; p < 0.01). For arterial and venous procedures combined, uninterrupted warfarin was associated with lower odds of access site hematoma (OR, 0.68; 95% CI: 0.51, 0.91;p = 0.01), bleeding complications (OR, 0.59; 95% CI: 0.48, 0.74; p < 0.01), ischemic stroke (OR, 0.25; 95% CI: 0.12, 0.50; p < 0.01), and major bleeding (OR, 0.61; 95% CI: 0.49, 0.77; p < 0.01). A random effects model with odds ratios was utilized to analyze acquired data.
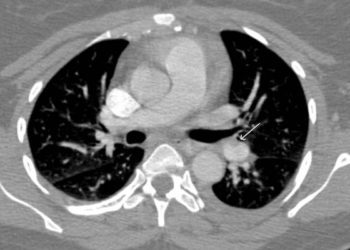
Image: PD
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.