2 Minute Medicine Rewind August 8, 2022
1. Transcranial direct current stimulation improved inattention symptoms in adult patients with ADHD, with no significant adverse effects.
Evidence Rating Level: 1 (Excellent)
Attention-Deficit Hyperactivity Disorder (ADHD) is a neurodevelopmental condition for which pharmacotherapy is currently the first line treatment. While pharmacological treatment for ADHD is effective, patient adherence is often low, and as such, non-pharmacological options are needed. In this randomized clinical trial, 64 patients with psychiatrist-diagnosed ADHD were randomized to either the transcranial direct current stimulation (tDCS) group or sham group and were assessed for improvements in inattentive scores on a clinician-administered adult ADHD scale. The tDCS group underwent 30-minute daily sessions of self-administered and home-based tDCS for four weeks. Compared to the sham group, participants in the active tDCS group had improved inattention scores (23.63 and 18.88, respectively). A statistically significant result was identified based on the linear mixed-effects model (βinteraction -3.18, 95%CI, -4.60 to -1.75). No serious or severe adverse events were observed; milder adverse events included dizziness and depressive symptoms. In conclusion, this randomized control trial confirms the efficacy of daily tDCS sessions for adults with ADHD in reducing symptoms of inattention. However, as tDCS had minimal effects on other symptoms of ADHD such as hyperactivity-impulsivity, depression, and anxiety, other treatment methods may still be necessary as an adjuvant. As well, this study only included patients without significant comorbid psychiatric conditions which may alter these results and the efficacy of tDCS. Nevertheless, tDCS remains a novel therapeutic agent for ADHD and targeting inattention, without significant adverse effects on patients. As such, further research investigating this modality of treatment may be beneficial to patients with ADHD.
1. There was no significant difference in risk of motor vehicle accidents between patients with an emergency department presentation with syncope compared to matched controls.
Evidence Rating Level: 2 (Good)
Syncope, defined as a sudden loss of consciousness and postural tone, can incapacitate drivers and result in motor vehicle accidents. While some literature believes that syncope-related accidents are rare and driving restrictions following syncopal episodes are not warranted, others believe that more restrictions are required. As there is not yet a consensus on this controversial topic, this study aims to identify crash risk following emergency department presentation with a syncopal episode. In this retrospective cohort study, 9223 participants with visits to the emergency department in British Columbia, Canada for a syncopal episode and 34,366 matched controls were assessed for motor vehicle accidents following the hospital visit. The results show that there was no significant difference with regards to risk in motor vehicle accident between the syncope and control groups; 9.2% of patients experienced a crash in the syncope group versus 10.1% in the control group (aHR 0.93, 95%CI 0.87-1.01). In conclusion, no evidence of increased crash risk following a syncopal episode was identified, which may suggest that current driving restrictions and guidelines following a first-episode syncope are already well delineated. However, there are several factors that must be taken into consideration prior to interpreting these results. For instance, individuals may be more reluctant to drive and may be informed by their physicians to avoid driving following the syncopal incident, which can naturally reduce motor vehicle crash risk. Additionally, while this study utilized a straight-forward design and obtained objective data to assess accident risk, it still has limitations. Firstly, this study did not discern specific causes for syncopal episodes in these patients and varying etiologies may have different risks of syncope recurrence. Moreover, the participants’ pre-existing comfort and experience with driving were not identified. This study’s generalizability is also limited as participants were only recruited from British Columbia. Nevertheless, given the controversy surrounding driving regulations and syncopal episodes, these findings do warrant further research and investigation.
1. Ciprofol was just as effective to propofol for general anesthesia induction in patients undergoing gynecological surgery and presents fewer adverse events.
Evidence Rating Level: 1 (Excellent)
In anesthesia practice, propofol is traditionally used to induce and maintain general anesthesia. While it does have a strong utility, propofol also may cause several adverse effects such as the inhibition of the circulatory and respiratory systems. As such, alternative drug choices for general anesthesia are needed. Ciprofol is a newly developed, short-acting GABA receptor which has been thought to be more potent than propofol with minor residual side effects, although there is limited data available regarding its use. This randomized control trial aims to investigate the safety and efficacy of ciprofol when used to induce general anesthesia in individuals undergoing gynecological surgery, compared to propofol. A total of 120 women planned for gynecological surgery were randomly assigned to either ciprofol or propofol groups, and success rate of general anesthesia induction was assessed. The results of this study identified no significant differences between the ciprofol and propofol groups with regards to onset of successful anesthetic induction (35.4 vs 34.8, respectively). Additionally, for patients in the ciprofol group, blood pressure values decreased significantly less compared to the propofol group, suggesting a less adverse effect on the cardiovascular system. In conclusion, ciprofol is non-inferior to propofol when used for the induction of general anesthesia and poses less serious adverse events. However, this study continues to be limited as participants with pre-existing respiratory or cardiovascular conditions were not included in the study and the sample size was limited. As well, this study only examined patients undergoing gynecological surgery; however, patients undergoing other types of surgery may respond differently to these anesthetics. Nevertheless, as the findings of this study do support the efficacy and safety of ciprofol, further research is warranted.
Nonsteroidal Anti-Inflammatory Drug Exposure and the Risk of Microscopic Colitis
1. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) were independently associated with the development of microscopic colitis.
Evidence Rating Level: 2 (Good)
Microscopic colitis, a type of chronic inflammatory bowel disease, is a common cause of abdominal pain and chronic diarrhea. In recent years, the incidence of microscopic colitis has significantly increased to levels comparable to Crohn’s disease and ulcerative colitis. It has been suggested that medications such as non-steroidal anti-inflammatory drugs (NSAIDs), proton-pump inhibitors (PPIs), and selective serotonin reuptake inhibitors (SSRIs) can contribute to the onset of microscopic colitis; however, the evidence behind this remains unclear. In this prospective cohort study, 144 patients prospectively evaluated for chronic diarrhea underwent colonoscopic evaluation and were assessed for their medication use and evidence of microscopic colitis on colonoscopy, in attempt to investigate the potential association between drug exposure and microscopic colitis. From these included patients, microscopic colitis was identified in a total of 80 individuals. Of these patients diagnosed, the use of aspirin and other NSAIDs was higher compared to those that were not diagnosed with microscopic colitis (OR 3.04, 95%CI 1.65-5.69). In conclusion, this study confirms that the use of NSAIDs is likely associated with the onset of microscopic colitis. Strengths of this study include its prospective design and use of a control group who had a similar presentation. However, this study remains limited due to its single center patient enrollment reducing generalizability to the broader population. As well, medication use data was obtained from patients through surveys, which may be not entirely accurate. Despite this, further research investigating medication use and its effect on the development of microscopic colitis should be conducted, considering the findings of this study.
1. Among hospitalized patients, methamphetamine use was associated with an increased risk of cardiovascular disease.
2. Among individuals using methamphetamines, those with chronic kidney disease, hypertension, and diabetes had an increased risk of cardiovascular disease.
Evidence Rating Level: 2 (Good)
Methamphetamine use is growing to be a global health crisis and presents a significant disease burden. Studies have suggested that methamphetamine use is associated with cardiovascular disease (CVD) and worse outcomes, although there is limited evidence exploring the incidence and predictors of CVD among individuals using amphetamines. In this retrospective cohort study, data from 202,490,246 Californian patients between 2005 and 2011 was obtained to assess hospital admissions, methamphetamine use, and incidence of pulmonary hypertension, stroke, heart failure, myocardial infarction, and overall CVD burden. The results of this study suggest that the incidence of CVD was 32% higher among individuals who used methamphetamines compared to those who did not (HR 1.32, 95%CI 1.26-1.38). Specifically, methamphetamine use was associated with elevated risk of heart failure, myocardial infarction, pulmonary hypertension, and stroke. Factors contributing to an increased risk of developing CVD among methamphetamine users included chronic kidney disease (HR 2.38, 95%CI 1.74-3.25), a pre-existing diagnosis of hypertension (HR 2.26, 95%CI 2.03-2.51), diabetes (HR 1.75, 95%CI 1.55-1.97), and smoking (HR 1.28, 95%CI 1.17-1.40). Interestingly, the simultaneous use of cocaine and alcohol were not associated with an increased risk of CVD overall, among methamphetamine users. In conclusion, methamphetamine use presents a significant healthcare burden globally due to the risks associated with cardiovascular disease. This study had several strengths including the longitudinal nature with follow-up of selected participants over many years. As well, a large and diverse population was selected, which improves the power and overall validity of the study. Further research investigating the mechanisms of action behind the association of cardiovascular disease with methamphetamine use, as well as the effects of different types of amphetamines along with the effects of its duration of use and dosage, could be very valuable.
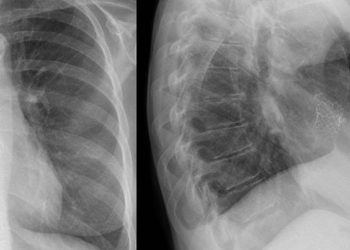
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.