2 Minute Medicine Rewind May 26, 2025
Exposure Therapy in Mixed Reality for Obsessive-Compulsive Disorder: A Randomized Clinical Trial
1. In this randomized clinical trial, mixed reality exposure and response prevention (MERP) was a feasible treatment for contamination obsessive-compulsive disorder (C-OCD); however, it did not significantly outperform self-guided exposure response prevention (SERP).
Evidence Rating Level: 1 (Excellent)
Obsessive-compulsive disorder (OCD) is a mental health disorder affecting 1-3% of individuals worldwide. The first line recommended treatment for OCD is cognitive behavioural therapy (CBT) with exposure and response prevention (ERP). Although this is the treatment with the best evidence in prior literature, its use in practice remains limited. Exposure therapy in virtual reality (VR) is a novel way to treat patients under optimal conditions, however, the research on EPR in VR (VERP) is limited. To assess this research gap, this randomized clinical trial (RCT) aimed to evaluate the efficacy of ERP in mixed reality (MERP) by comparing it to an active control group, namely self-guided ERP (SERP), in patients with contamination OCD (C-OCD). Assessments were conducted at baseline, 6 weeks, and 3 months post-treatment. Participants were randomized 1:1 into either the MERP or SERP group. The MERP sessions were conducted once a week for 6 weeks, with each one lasting between 60 and 90 minutes. The SERP participants were instructed to follow 1 self-guided exercise per week for 4 weeks, selecting real objects for their ERPs. To assess the severity of OCD symptoms, the Yale-Brown Obsessive Compulsive Scale (Y-BOCS) was used. A total of 36 participants (mean [SD] age 35.42 [14.03]) were included, with 18 in each group. Severe OCD symptoms were present in both groups, with the baseline Y-BOCS score slightly higher in the MERP group compared to the SERP group (26.94 vs. 24.22). The most common comorbid diagnosis was major depressive disorder (23 [63.9%]). The post-intervention and follow-up assessments were completed by 29 participants (80.6%). The MERP and SERP groups showed comparable reductions in OCD symptoms (Y-BOCS) with mean differences of 3.15 and 1.47, respectively, np² = 0.002; 95% CI, -3.187 to 3.893). The MERP group significantly improved from baseline to post-treatment (Cohen d, 0.584-0.931; 95% CI, 0.026-1.551). This randomized clinical trial found that MERP may be a promising treatment for C-OCD however, there was no significant advantage over SERP.
1. In this cohort of older adults, the overall incidence of dementia decreased from 2015 to 2021, however, the prevalence increased.
Evidence Rating Level: 2 (Good)
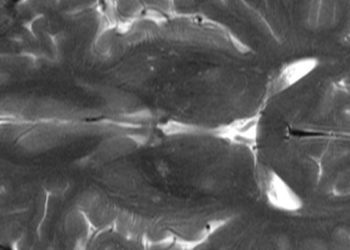
Dementia has become a top priority in the United States due to the rapidly aging population. Dementia is a group of neurological conditions characterized by a decline in cognitive function that interferes with daily life. The burden of disease disproportionately impacts marginalized communities, specifically Black Americans and those with a lower socioeconomic status. This study aimed to assess how dementia rates vary by sex, race, and neighborhood deprivation using Medicare data, to inform future policies. To best achieve this, a retrospective population-based cohort study was conducted using Medicare claims data from 2013 to 2021 to analyze dementia rates in older adults. Researchers included only those enrolled in traditional fee-for-service Medicare, excluding those with private health plans. The primary outcomes were the rates of dementia incidence and prevalence adjusted for age and sex. Between 2015 to 2021, there were 5,025,039 new cases of dementia reported. The number of cases decreased from 838,824 to 628,902, with age and sex-adjusted incidence rates decreasing from 3.5% to 2.8%. During this same period, prevalence increased, reaching the highest point in 2019 with 3,140,758 cases before slightly declining to 2,875,718 by 2021, corresponding to an increase from 10.5% to 11.8%. In 2015, men had a statistically significantly higher rate of dementia than women (3.5% vs. 3.4%). By 2021, the difference had grown further (2.9% vs. 2.6%; estimated difference-in-difference 0.94, 95% confidence interval (CI) 0.94 to 0.95; P<0.001). In 2015, the highest age- and sex-adjusted incidence rates of dementia were in black beneficiaries (4.2%, 95% CI 4.2% to 4.2%), followed by Hispanic beneficiaries (3.7%, 3.6% to 3.7%), and non-Hispanic white beneficiaries (3.4%, 3.4% to 3.5%). In 2021, black beneficiaries still had the highest incidence (3.1%), followed by non-Hispanic white beneficiaries (2.8%) and then Hispanic beneficiaries (2.6%). The gap in dementia rates between white beneficiaries and other racial and ethnic groups decreased significantly between 2015 and 2021 (estimated difference-in-difference 0.92 (95% CI 0.91 to 0.93) compared with black beneficiaries, 0.88 (0.87 to 0.89) compared with Hispanic beneficiaries). In this retrospective cohort study from 2015 to 2021, the incidence of dementia decreased, however, the prevalence significantly increased, indicating that by 2021, approximately 2.9 Medicare beneficiaries likely had a dementia diagnosis.
1. In this multicenter randomized controlled trial, a 12-week personalized visual perceptual learning (VPL) program significantly improved visual field function in stroke patients with visual field defects (VFDs) compared to no treatment.
Evidence Rating Level: 1 (Excellent)
Brain damage, such as from a stroke, can cause visual field defects (VFDs) that reduce vision and impair quality of life, with limited spontaneous recovery beyond three months. These usually affect the same side of the visual field in both eyes, and depending on where the damage is, may block a quarter (quadrantanopia) or half (hemianopia) of what a person can see. Current treatment strategies include compensation, substitution, and restitution, but no approach has been proven effective in randomized trials. Visual perceptual learning (VPL) is a promising therapy using repetitive training to improve vision in the blind field. This multicenter randomized clinical trial compared 12 weeks of personalized VPL training to no training to assess the impact of visual recovery in patients with chronic stroke-related VFDs. Participants were randomly assigned 1:1 to either the training or control group. To assess visual fields, the Humphrey visual field (HVF) test was conducted at baseline and 12-week follow-up. The final sample included 82 participants, with 41 in the training group and 41 in the control group (median [IQR] age 52 [42-65] years). Over the 12 weeks, the training group experienced significantly greater improvement than the control group in the visual field and the damaged half. In the full field, the median improvement was 72 degrees squared (95% CI, 36-108; P=.003), with average improvements of 194.1 [SD 197.3] vs 82.5 [SD 95.0] degrees squared. In the damaged hemifield, the median improvement was also 72 degrees squared (95% CI, 36-108; P=.002) with average improvements of 158.9 (SD 159.0) vs 72.0 (91.4) degrees squared. All improvements reflected sensitivity gains of at least 6 dB. In summary, this randomized clinical trial proved that VPL led to significant improvements in both overall and damaged visual fields in people with long-term VFDs after stroke.
1. In this Australian cohort of adults, individuals diagnosed with cancer experienced greater declines in physical functioning and slightly higher psychological distress compared to people without cancer
2. This finding was especially pronounced among those with advanced disease or recent treatment.
Evidence Rating Level: 1 (Excellent)
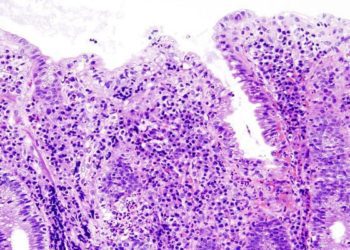
Cancer survival rates are improving worldwide due to better early detection and treatment. In Australia, the 5-year survival rate for all cancers rose from 50.2% in 1989-1993 to 70.6% in 2015-2019. While cancer survivors are generally more likely to experience physical limitations and mild psychological distress, outcomes vary widely by cancer type, stage, and treatment status. Previous research has been limited by short follow-up periods, a focus on single cancer types, and a lack of pre-diagnosis data or control groups without cancer. This study addresses those gaps by using large-scale, population-based data to compare physical and psychological changes from before to after cancer diagnosis with matched changes in people without cancer. After removing ineligible individuals who had cancer at baseline, the main focus was on those who were newly diagnosed with cancer between the first and follow-up surveys. The primary outcomes were how much physical limitations (assessed using the Medical Outcomes Study Physical Functioning [MOS-PF] score) and psychological distress (assessed using the Kessler-10 [K10]) changed between baseline to follow-up. After meeting eligibility criteria, 142,682 participants were included in the study. Over 5.2 years, 9,313 participants were diagnosed with cancer while 133,369 were not. Participants diagnosed with cancer experienced a greater deterioration in physical function over time compared to those without cancer (40.6% vs. 52.3%). Compared to people without cancer, cancer survivors had larger declines in physical functioning (average follow-up score: 77.5 vs 82.9; average change: -8.31 vs -4.71; adjusted difference -2.55, 95% CI: -2.97 to -2.13) and slightly more psychological distress (average follow-up score: 13.6 versus 13.5 at follow-up; mean-change: 0.24 versus − 0.04; adjusted-difference 0.21 (95%CI = 0.12–0.31)). Physical health declined more for people with multiple myeloma, lung cancer, and leukemia, and less for those with breast, colorectal, or prostate cancer. Survivors with advanced disease or those still undergoing treatment experienced greater declines in physical and psychological well-being. However, psychological well-being was similar between cancer-free individuals and survivors who were not receiving treatment at follow-up. In conclusion, participants newly diagnosed with cancer experienced a significantly greater decline in physical function and slightly decreased psychological well-being compared to participants without cancer.
1. In this prospective cohort study, social isolation is associated with decreased survival time and accelerated onset of cardiovascular disease (CVD) in individuals with chronic kidney disease (CKD).
Evidence Rating Level: 1 (Excellent)
Chronic kidney disease (CKD) is a condition where the kidney has abnormalities in structure or function lasting for 3 months or longer. The incidence of CKD is rising globally and is expected to increase further within the next 15 years. As CKD progresses to end-stage, it requires extensive medical care and increases the risk of serious health complications. Managing CKD focuses on identifying risk factors, slowing disease progression and preventing cardiovascular mortality. Social isolation is a recognized but often overlooked factor that can negatively impact health, increasing the risk of health issues, including cardiovascular disease (CVD) and death. While social isolation has been linked to faster kidney function decline in the general population, its impact on outcomes in people already living with CKD is unclear. To address this research gap, this prospective cohort study sought to evaluate the relationship between social isolation and CVD and mortality among patients with CKD. Participants with CKD at baseline between the ages of 40 and 69 years were recruited through the UK Biobank. Social isolation was assessed through self-reported questionnaires. The total sample included 13,090 participants (mean age 65 [IQR 61-68] years), with 62% having a decreased estimated glomerular filtration rate (eGFR). Individuals experiencing moderate and high levels of social isolation showed accelerated all-cause mortality (time ratio 0.87 [95% CI, 0.82-0.93; P<0.001] and 0.76 [95% CI, 0.70-0.82; P<0.001] respectively) compared to those experiencing the least isolation. Moderate and high levels of social isolation were minimally associated with accelerated CVD mortality, with time ratios of 0.93 (95% CI, 0.87-0.99; P=0.039) and 0.87 (95% CI, 0.79-0.96; P=0.005), respectively. However, this association was observed for stroke but not for coronary artery disease. In summary, social isolation was significantly associated with decreased survival time and accelerated onset of CVD, specifically stroke, in individuals with CKD.
Image: PD
©2025 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.