2 Minute Medicine Rewind November 2 – November 8, 2015
Isosorbide Mononitrate in Heart Failure with Preserved Ejection Fraction
Few medications have been shown to improve mortality or quality of life in patients with congestive heart failure with preserved ejection fracture. Nitrates have been postulated to improve activity tolerance in such patients. In this multicenter, double-blind, cross-over study, 110 patients with congestive heart failure with preserved ejection fraction were randomized to either 6 weeks of escalating doses of isosorbide mononitrate or placebo and assessed for daily activity level. Activity level was quantified by daily patient-worn accelerometer activity when patients were taking the max dose (120mg) of isosorbide mononitrate or placebo. In this study, there was a trend towards lower daily activity in patients receiving isosorbide mononitrate (-381 accelerometer units, 95% CI: -780 to 17, p = 0.06) and there was no difference in 6-minute walk difference, quality-of-life, or NT-proBNP levels. In this study, there did not appear to be benefit for patients with congestive heart failure with preserved ejection fraction to take isosorbide mononitrate with respect to quality-of-life or activity level.
Effect of Financial Incentives to Physicians, Patients, or Both on Lipid Levels
Decisions can be influenced by financial incentives and have been trialed in healthcare maintenance and prevention. Both physician and patient level financial incentives can affect patient healthcare decisions. In this multicenter, 2:2 design cluster-randomized clinical trial, 1503 patients with high Framingham Risk Score (>20%) of 340 providers were randomized to either physician incentives, patient incentives, shared physician and patient incentives, or none and were assessed at 12 months to identify progress inreaching LDL cholesterol goals. The shared physician and patient incentives group achieved a mean reduction of LDL-C of 33.6 mg/dL (95% CI: 30.1 to 37.1) while the physician incentives group achieved a mean reduction of 27.9 mg/dL (95% CI: 24.9 to 31.0) and the patient incentives group and control group both achieved a mean reduction of 25.1 mg/dL (95% CI: 21.6-28.5). Only patients in the shared physician and patient incentives group achieved reductions statistically significantly different from the control group (difference of 8.5 mg/dL, 95% CI 3.8 – 13.3, p = 0.002). This difference, however, is clinically modest and is unclear if this approach generalizable to longer periods of time or can result in clinically significant difference in outcomes.
Weight loss and Health status 3 Years after Bariatric Surgery in Adolescents
Bariatric surgery has been shown to improve objective metrics of glucose control, blood pressure management, and weight loss in adult patients with severe obesity. Bariatric surgery is increasingly being considered in younger patients with severe obesity. In this prospective cohort study of 242 adolescent patients at 5 American centers, patients who underwent either Roux-en-Y gastric bypass or sleeve gastrectomy were evaluated through three years after the procedure. Three years after the procedure, mean weight decreased by 27% (95% CI: 25 to 29), 95% (95% CI: 85 to 100%) of patients had remission of type 2 diabetes, 76% (95% CI: 72 to 100%) of patients had remission of abnormal kidney function, and 66% (95% CI: 57 to 74%) of patients had remission of dyslipidemia. Thirteen percent (95% CI: 9 to 18%) of patients had additional intraabdominal procedures and 57% (95% CI: 50 to 65%) of patients had low serum iron. In this study, there were significant improvements in weight, cardiovascular risk factor mediation, and quality of life in patients who underwent bariatric surgery, however complications include nutritional deficiencies and need for further abdominal procedures.
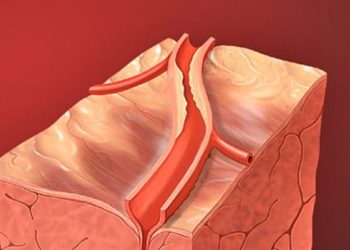
Fractional flow reserve (FFR) has been thought to be a useful supplement to conventional angiography to identify culprit and symptomatic coronary artery atherosclerosis. The Fractional Flow Reserve Versus Angiography for Multivessel Evaluation (FAME) study identified opportunities to perform fewer stents while having equivalent to superior clinical outcomes as patients randomized to the FFR group only had percutaneous intervention (PCI) performed if FFR was less than 80%. During the trial, the number of stents placed per patient was statistically decreased in the FFR group (1.9 vs. 2.7, p < 0.0001). At five year outcome analysis, there was no statistically significant difference in major adverse cardiac events (28% vs. 31%, RR 0.91, 95% CI: 0.75 – 1.10, p = 0.31). This long term follow-up reaffirms the long term use of FFR to decrease the number of PCI stents placed and optimize resource utilization.
Trastuzumab has been known to have cardiotoxicity and surveillance echocardiography has been routine to assess for asymptomatic and symptomatic left ventricular ejection fraction (LVEF). In this retrospective analysis of a multicenter trial enrolling 406 patients with node-negative, ERBB2-positive breast cancer and normal baseline cardiac function, the investigators reviewed the incidence and frequency of left ventricular systolic dysfunction. Study patients recieved weekly 80mg/m2 doses of paclitaxel and trastuzumab for 12 weeks followed by 39 weeks of trastuzumab alone. In this study, 2 patients (0.5%, 95% CI: 0.1 to 0.8%) developed symptomatic left ventricular dysfunction requiring investigators to stop trastuzumab and 13 (3.2%, 95% CI 1.9% to 5.4%) had significant but asymptomatic decrease in LVEF. Of the patients with asymptomatic LVEF reduction, 11 completed study treatment. In this retrospective analysis, the incidence of cardiomyopathy secondary to trastuzumab was low, suggesting routine LVEF monitoring can be reduced.
Image: PD
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.